Enhanced S-cone Syndrome: an NR2E3-Associated Retinal Dystrophy
Home / Retina and Vitreous / Hereditary and Choroidal Dystrophies
Title: Enhanced S-cone Syndrome: an NR2E3-Associated Retinal Dystrophy
Authors: Aniket Ramshekar, PhD, MSIV, University of Utah School of Medicine and Cecinio “Nikko” Ronquillo, MD, PhD
Date: 8/23/23
Keywords/Main Subjects: enhanced s-cone syndrome, NR2E3, NRL, nyctalopia, photoreceptors
Diagnosis: Enhanced S-cone Syndrome
Description of Case: A 13-year-old male presented with impaired nighttime vision (i.e., nyctalopia) and peripheral vision loss. Past ocular history is notable for glasses since he was 4 years old. Medical and developmental history were unremarkable. Family history was unremarkable.
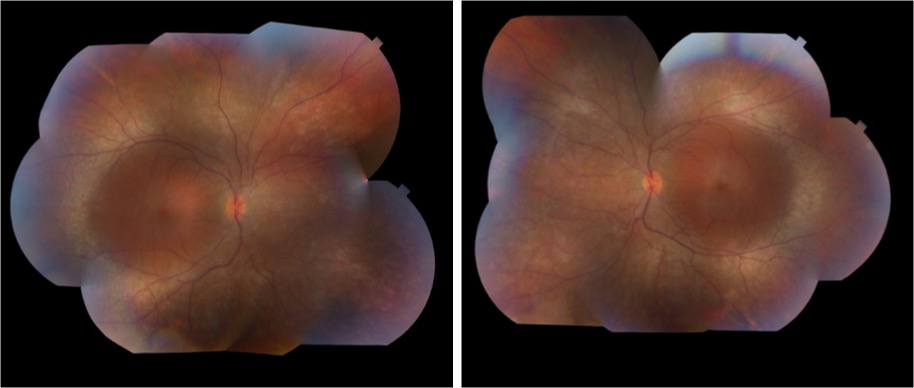
On exam, the patient had best corrected visual acuity (BCVA) of 20/30 OD and 20/40 OS, intraocular pressure (IOP) of 12 OD and 9 OS, and reduced peripheral vision to confrontation OU. Fundus exam was notable for loss of pigment, grayish appearance around the arcades and peripheral retina associated with nummular pigment changes along the superior arcade OS (Figure 1).
Fundus autofluorescence revealed hyper-autofluorescent spots surrounding the fovea OU (Figure 2).
Optical coherence tomography (OCT) demonstrated retained inner layers of the retina OU, cystic changes in the outer plexiform layer (OPL) OU, and loss of definition of the outer retinal layers OU (Figure 3).
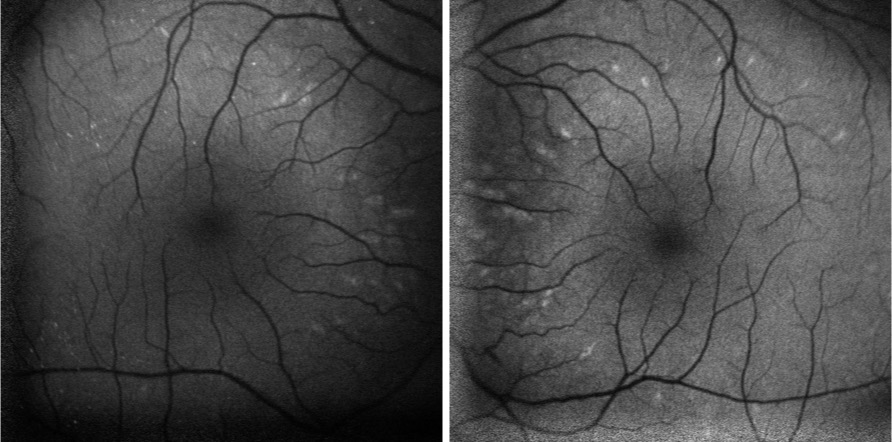
Goldmann visual field exam was full (Figure 4).
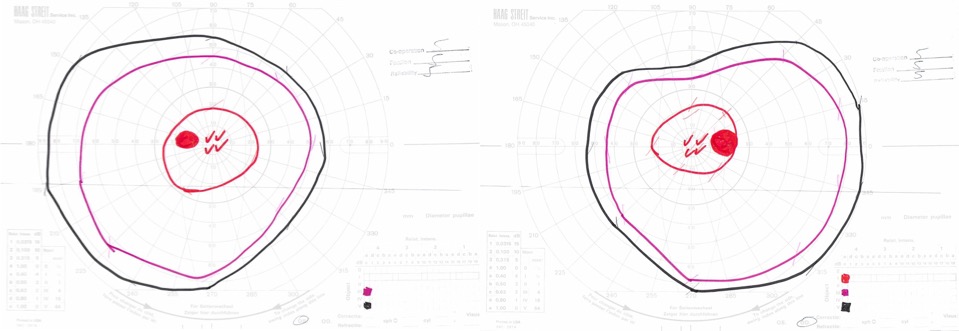
Full-field electroretinogram (ERG) showed diminished scotopic and photopic bright white flashes OU and 30 Hz flicker response that was delayed and diminished in amplitude OU (Figure 5).
Given the concern for inherited retinal dystrophy, the patient was referred for genetic testing that revealed a homozygous NR2E3 c.119-2A>C variant, which disrupts the nearby universal “AG” splice acceptor site and is likely pathogenic.
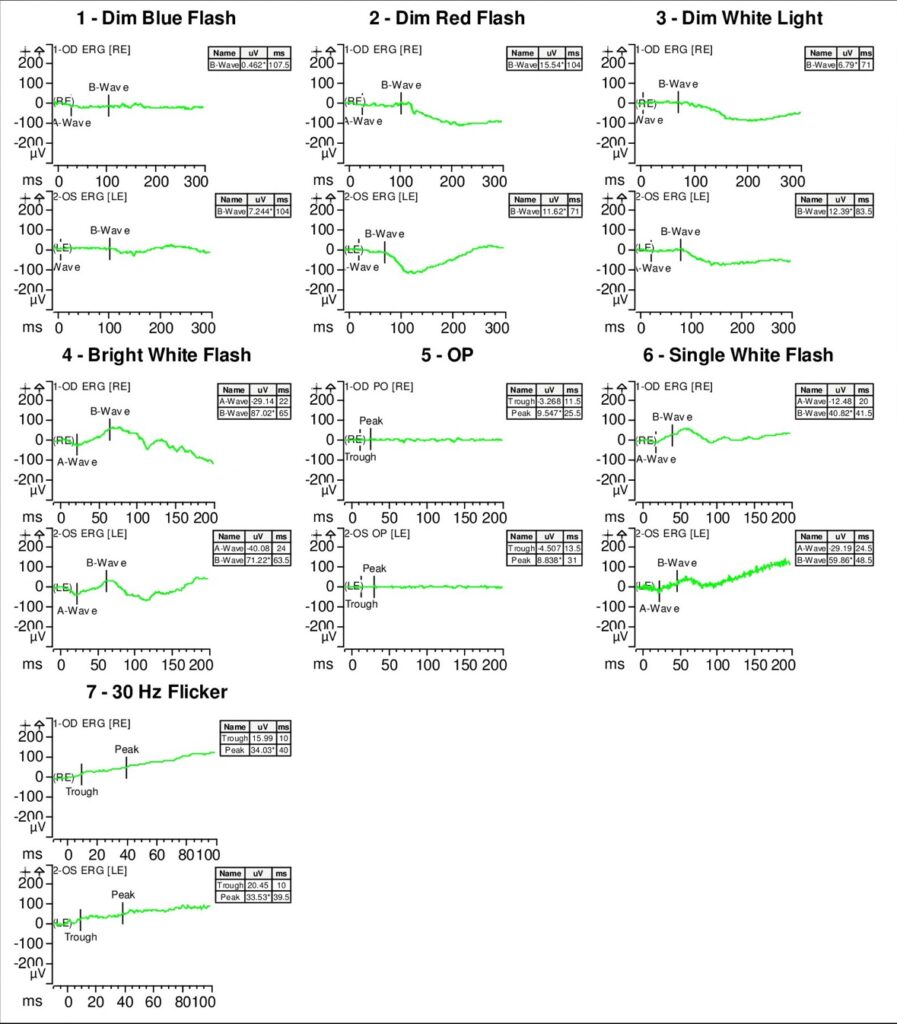
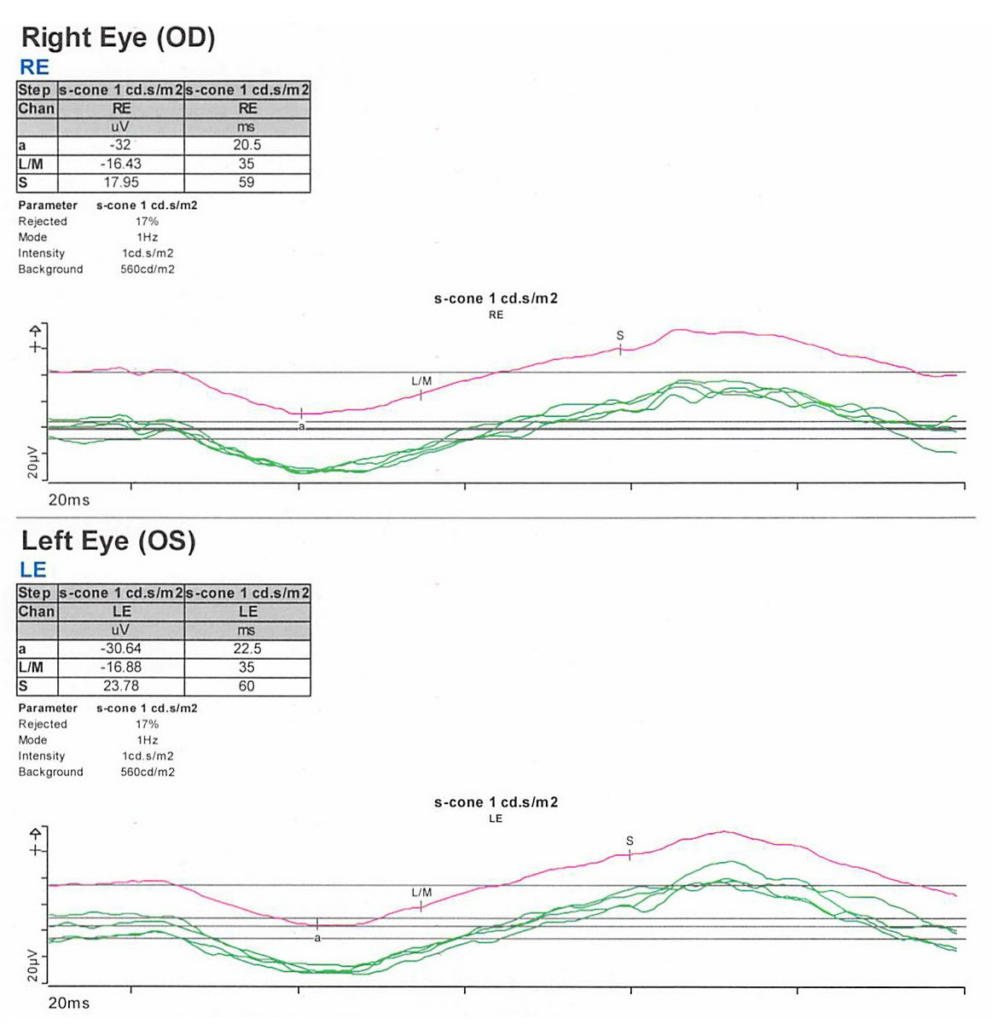
S-cone ERG, acquired in response to a blue wavelength on an orange wavelength background, demonstrated a greater than anticipated response OU (Figure 6).
Epidemiology: Enhanced S-cone syndrome (ESCS) is a rare inherited progressive retinal degeneration. The prevalence of ESCS is not well-established; however, studies have found gene mutations associated with ESCS worldwide.1-12
Genetics: ESCS is inherited in an autosomal recessive pattern. NR2E3 (Nuclear Receptor Subfamily 2, Group E, Member 3) mutations are primarily implicated in ESCS. There are over 30 pathogenic mutations in NR2E3 that have been associated with ESCS.13-15 In the United States, however, the NR2E3 c.119-2A>C variant is the most common.16
Some ESCS cases have also documented NRL (neural retina leucine zipper) mutations.17-20
Pathophysiology: NR2E3 protein is a retinal orphan nuclear receptor, a transcription factor expressed in the outer nuclear layer of the human retina.13 To gain mechanistic insights, NR2E3 mutations in mouse models have been shown to disrupt the development of rod photoreceptors and disrupt the differentiation of cone photoreceptors to L/M-cones leading to over-expansion of the S-cone population in the retina.21-23 NR2E3 expression is under the direct regulation of the transcription factor, NRL protein.24 Therefore, mutations in NRL lead to ESCS by affecting NR2E3 expression.25
Clinical presentation: The clinical presentation of ESCS is variable; however, listed below are some documented symptoms.26-28
- Night blindness (nyctalopia, due to reduced functioning rod photoreceptors)
- Increased sensitivity to blue light (due to the over-expansion of functioning S-cones)
- Reduced visual acuity
- Abnormal color vision, with a tendency to see colors as more vibrant or intense
Diagnosis: Given that the clinical presentation of ESCS is variable, the diagnostic testing might also demonstrate variable findings among patients. Below are some diagnostic findings associated with each clinical test:
- Fundus exam – Fundus exam might demonstrate torpedo-like lesions primarily located along the vascular arcades, subretinal fibrosis, nummular pigmentary changes along the vascular arcades, or intraretinal yellow dots.6,29
- ERG – full-field ERG might demonstrate a diminished rod response and similar waveform in response to both scotopic and photopic conditions. The 30 Hz flicker responses might demonstrate significantly delayed responses with attenuated amplitudes. With orange background, increased response to short wavelength (blue) might be elicited. The multifocal ERG (mfERG) might show preserved central responses, though can be delayed.6,30-35
- OCT – OCT might demonstrate cystoid macular edema (CME) or foveomacular schisis.31 There are some documented cases of subretinal fibrosis secondary to choroidal neovascularization that might also be detected by OCT.6,35-27 There was also a case of macular retinal vascularization of the posterior pole that was detected by OCT.38
- FA – In the peripheral retina, FA might demonstrate hypo-autofluorescence with patchy areas of advanced hypo-autofluorescence. In the macula, hyper-autofluorescent flecks have been documented.6 FA might also identify vascular changes (i.e., retinal or choroidal neovascularization) and complement OCT findings.
- Genetic testing can identify mutations in the NR2E3 or NRL genes and confirm the diagnosis
Differential diagnosis: Nyctalopia has a broad differential and includes conditions such as Vitamin A deficiency, cataracts, autoimmune retinopathy, glaucoma, and other inherited retinal dystrophies (i.e., congenital stationary night blindness, Oguchi’s disease, fundus albipunctatus). Therefore, a careful workup is required to narrow the differential to treat patients appropriately.
Some NR2E3 mutations are implicated in autosomal dominant retinitis pigmentosa, Goldmann-Favre syndrome, and clumped pigmentary retinal degeneration.39-41 Characterizing the underlying disease caused by the NR2E3 mutations might not improve medical management but would inform genetic counseling.
Management: There are currently no approved therapies to treat ESCS. However, CRISPR/Cas9 gene editing has been used preclinically to correct the homozygous NR2E3 c.119-2A>C splice site variant in induced pluripotent stem cells (iPSCs) from two patients with ESCS.42 This finding suggests that CRISPR/Cas9 gene editing might be a plausible treatment approach for ESCS in the future.
Current medical management includes treating foveomacular schisis and CME with carbonic anhydrase inhibitors, while choroidal neovascularization is treated with agents that inhibit vascular endothelial growth factor.43-49 Genetic testing and patient support programs should also be offered in all patient cases. Genetic penetrance and carrier frequency of the NR2E3 mutations are not well understood given the rarity of disease phenotypes. Therefore, genetic testing of the patient and family might help provide further information to improve genetic counseling.
Summary of the Case:
- ESCS is a rare inherited progressive retinal degenerative disease of the photoreceptors that can present as nyctalopia
- There is clinical and diagnostic variability among patients with ESCS, but mutations in the transcription factors, NR2E3 or NRL, are implicated in pathology
- Current treatment is limited to treating foveomacular schisis and CME with carbonic anhydrase inhibitors, and choroidal neovascularization with anti-VEGF agents
- Genetic testing should be offered to inform genetic counseling
- Studies exploring CRISPR/Cas9 gene editing show promise for future therapies
References
- Bandah, D., Merin, S., Ashhab, M., Banin, E. & Sharon, D. The spectrum of retinal diseases caused by NR2E3 mutations in Israeli and Palestinian patients. Arch Ophthalmol 127, 297-302, doi:10.1001/archophthalmol.2008.615 (2009).
- Gao, F. J. et al. Genetic and Clinical Findings in a Large Cohort of Chinese Patients with Suspected Retinitis Pigmentosa. Ophthalmology 126, 1549-1556, doi:10.1016/j.ophtha.2019.04.038 (2019).
- Alsalamah, A. K., Khan, A. O., Bakar, A. A., Schatz, P. & Nowilaty, S. R. Recognizable Patterns of Submacular Fibrosis in Enhanced S-Cone Syndrome. Ophthalmol Retina 5, 918-927, doi:10.1016/j.oret.2021.03.014 (2021).
- Habibi, I. et al. Different Phenotypes in Pseudodominant Inherited Retinal Dystrophies. Front Cell Dev Biol 9, 625560, doi:10.3389/fcell.2021.625560 (2021).
- Al-Khuzaei, S. et al. Novel Pathogenic Sequence Variants in NR2E3 and Clinical Findings in Three Patients. Genes (Basel) 11, doi:10.3390/genes11111288 (2020).
- de Carvalho, E. R. et al. Enhanced S-Cone Syndrome: Spectrum of Clinical, Imaging, Electrophysiologic, and Genetic Findings in a Retrospective Case Series of 56 Patients. Ophthalmol Retina 5, 195-214, doi:10.1016/j.oret.2020.07.008 (2021).
- Hebbar, P. et al. Genetic risk variants for metabolic traits in Arab populations. Sci Rep 7, 40988, doi:10.1038/srep40988 (2017).
- Van Cauwenbergh, C. et al. Mutations in Splicing Factor Genes Are a Major Cause of Autosomal Dominant Retinitis Pigmentosa in Belgian Families. PLoS One 12, e0170038, doi:10.1371/journal.pone.0170038 (2017).
- Kuniyoshi, K. et al. New truncation mutation of the NR2E3 gene in a Japanese patient with enhanced S-cone syndrome. Jpn J Ophthalmol 60, 476-485, doi:10.1007/s10384-016-0470-0 (2016).
- Kannabiran, C., Singh, H., Sahini, N., Jalali, S. & Mohan, G. Mutations in TULP1, NR2E3, and MFRP genes in Indian families with autosomal recessive retinitis pigmentosa. Mol Vis 18, 1165-1174 (2012).
- Udar, N., Small, K., Chalukya, M., Silva-Garcia, R. & Marmor, M. Developmental or degenerative–NR2E3 gene mutations in two patients with enhanced S cone syndrome. Mol Vis 17, 519-525 (2011).
- Naik, A. et al. Enhanced S-cone syndrome: Clinical spectrum in Indian population. Indian J Ophthalmol 67, 523-529, doi:10.4103/ijo.IJO_1480_18 (2019).
- Haider, N. B. et al. Mutation of a nuclear receptor gene, NR2E3, causes enhanced S cone syndrome, a disorder of retinal cell fate. Nat Genet 24, 127-131, doi:10.1038/72777 (2000).
- Schorderet, D. F. & Escher, P. NR2E3 mutations in enhanced S-cone sensitivity syndrome (ESCS), Goldmann-Favre syndrome (GFS), clumped pigmentary retinal degeneration (CPRD), and retinitis pigmentosa (RP). Hum Mutat 30, 1475-1485, doi:10.1002/humu.21096 (2009).
- Escher, P. et al. Mutations in NR2E3 can cause dominant or recessive retinal degenerations in the same family. Hum Mutat 30, 342-351, doi:10.1002/humu.20858 (2009).
- Stone, E. M. et al. Clinically Focused Molecular Investigation of 1000 Consecutive Families with Inherited Retinal Disease. Ophthalmology 124, 1314-1331, doi:10.1016/j.ophtha.2017.04.008 (2017).
- Iarossi, G. et al. A Novel Autosomal Recessive Variant of the NRL Gene Causing Enhanced S-Cone Syndrome: A Morpho-Functional Analysis of Two Unrelated Pediatric Patients. Diagnostics (Basel) 12, doi:10.3390/diagnostics12092183 (2022).
- Newman, H. et al. Homozygosity for a Recessive Loss-of-Function Mutation of the NRL Gene Is Associated With a Variant of Enhanced S-Cone Syndrome. Invest Ophthalmol Vis Sci 57, 5361-5371, doi:10.1167/iovs.16-19505 (2016).
- Nishiguchi, K. M. et al. Recessive NRL mutations in patients with clumped pigmentary retinal degeneration and relative preservation of blue cone function. Proc Natl Acad Sci U S A 101, 17819-17824, doi:10.1073/pnas.0408183101 (2004).
- Littink, K. W. et al. Autosomal Recessive NRL Mutations in Patients with Enhanced S-Cone Syndrome. Genes (Basel) 9, doi:10.3390/genes9020068 (2018).
- Haider, N. B., Naggert, J. K. & Nishina, P. M. Excess cone cell proliferation due to lack of a functional NR2E3 causes retinal dysplasia and degeneration in rd7/rd7 mice. Hum Mol Genet 10, 1619-1626, doi:10.1093/hmg/10.16.1619 (2001).
- Haider, N. B. et al. Nr2e3-directed transcriptional regulation of genes involved in photoreceptor development and cell-type specific phototransduction. Exp Eye Res 89, 365-372, doi:10.1016/j.exer.2009.04.006 (2009).
- Haider, N. B. et al. The transcription factor Nr2e3 functions in retinal progenitors to suppress cone cell generation. Vis Neurosci 23, 917-929, doi:10.1017/S095252380623027X (2006).
- Oh, E. C. et al. Rod differentiation factor NRL activates the expression of nuclear receptor NR2E3 to suppress the development of cone photoreceptors. Brain Res 1236, 16-29, doi:10.1016/j.brainres.2008.01.028 (2008).
- Mears, A. J. et al. Nrl is required for rod photoreceptor development. Nat Genet 29, 447-452, doi:10.1038/ng774 (2001).
- Khan, A. O., Aldahmesh, M. & Meyer, B. The enhanced S-cone syndrome in children. BMJ Case Rep 2009, doi:10.1136/bcr.10.2008.1163 (2009).
- Fishman, G. A., Jampol, L. M. & Goldberg, M. F. Diagnostic features of the Favre-Goldmann syndrome. Br J Ophthalmol 60, 345-353, doi:10.1136/bjo.60.5.345 (1976).
- Garafalo, A. V. et al. Cone Vision Changes in the Enhanced S-Cone Syndrome Caused by NR2E3 Gene Mutations. Invest Ophthalmol Vis Sci 59, 3209-3219, doi:10.1167/iovs.18-24518 (2018).
- Yzer, S. et al. Expanded clinical spectrum of enhanced S-cone syndrome. JAMA Ophthalmol 131, 1324-1330, doi:10.1001/jamaophthalmol.2013.4349 (2013).
- Tsang, S. H. & Sharma, T. Enhanced S-Cone Syndrome (Goldmann-Favre Syndrome). Adv Exp Med Biol 1085, 153-156, doi:10.1007/978-3-319-95046-4_28 (2018).
- Vincent, A., Robson, A. G. & Holder, G. E. Pathognomonic (diagnostic) ERGs. A review and update. Retina 33, 5-12, doi:10.1097/IAE.0b013e31827e2306 (2013).
- Hood, D. C., Cideciyan, A. V., Roman, A. J. & Jacobson, S. G. Enhanced S cone syndrome: evidence for an abnormally large number of S cones. Vision Res 35, 1473-1481, doi:10.1016/0042-6989(95)98727-q (1995).
- Jacobson, S. G., Marmor, M. F., Kemp, C. M. & Knighton, R. W. SWS (blue) cone hypersensitivity in a newly identified retinal degeneration. Invest Ophthalmol Vis Sci 31, 827-838 (1990).
- Marmor, M. F., Jacobson, S. G., Foerster, M. H., Kellner, U. & Weleber, R. G. Diagnostic clinical findings of a new syndrome with night blindness, maculopathy, and enhanced S cone sensitivity. Am J Ophthalmol 110, 124-134, doi:10.1016/s0002-9394(14)76980-6 (1990).
- Audo, I. et al. Phenotypic variation in enhanced S-cone syndrome. Invest Ophthalmol Vis Sci 49, 2082-2093, doi:10.1167/iovs.05-1629 (2008).
- Nakamura, M. et al. Enhanced S-cone syndrome with subfoveal neovascularization. Am J Ophthalmol 133, 575-577, doi:10.1016/s0002-9394(01)01428-3 (2002).
- Zerbib, J. et al. Retinochoroidal Anastomosis Associated with Enhanced S-Cone Syndrome. Retin Cases Brief Rep 13, 295-299, doi:10.1097/ICB.0000000000000594 (2019).
- Bazvand, F., Khojasteh, H. & Zarei, M. Novel findings in enhanced S-cone syndrome: a case with macular retinal neovascularization and severe retinal vasculitis. Doc Ophthalmol 139, 221-226, doi:10.1007/s10633-019-09706-6 (2019).
- Sharon, D., Sandberg, M. A., Caruso, R. C., Berson, E. L. & Dryja, T. P. Shared mutations in NR2E3 in enhanced S-cone syndrome, Goldmann-Favre syndrome, and many cases of clumped pigmentary retinal degeneration. Arch Ophthalmol 121, 1316-1323, doi:10.1001/archopht.121.9.1316 (2003).
- Chavala, S. H. et al. An Arg311Gln NR2E3 mutation in a family with classic Goldmann-Favre syndrome. Br J Ophthalmol 89, 1065-1066, doi:10.1136/bjo.2005.068130 (2005).
- Gire, A. I. et al. The Gly56Arg mutation in NR2E3 accounts for 1-2% of autosomal dominant retinitis pigmentosa. Mol Vis 13, 1970-1975 (2007).
- Bohrer, L. R. et al. Correction of NR2E3 Associated Enhanced S-cone Syndrome Patient-specific iPSCs using CRISPR-Cas9. Genes (Basel) 10, doi:10.3390/genes10040278 (2019).
- Iannaccone, A., Fung, K. H., Eyestone, M. E. & Stone, E. M. Treatment of adult-onset acute macular retinoschisis in enhanced s-cone syndrome with oral acetazolamide. Am J Ophthalmol 147, 307-312 e302, doi:10.1016/j.ajo.2008.08.003 (2009).
- Chatzistergiou, V. et al. Optical Coherence Tomography Analysis of Cystoid Macular Edema in Retinal Dystrophy Treated with Oral Acetazolamide: Two Cases. Klin Monbl Augenheilkd 237, 484-486, doi:10.1055/a-1068-2762 (2020).
- Genead, M. A., Fishman, G. A. & McAnany, J. J. Efficacy of topical dorzolamide for treatment of cystic macular lesions in a patient with enhanced S-cone syndrome. Doc Ophthalmol 121, 231-240, doi:10.1007/s10633-010-9247-9 (2010).
- Hajali, M. & Fishman, G. A. Dorzolamide use in the management of macular cysts in a patient with enhanced s-cone syndrome. Retin Cases Brief Rep 3, 121-124, doi:10.1097/ICB.0b013e31818faa21 (2009).
- Bechet, L. et al. Management of a case of Enhanced S-cone syndrome with massive foveoschisis treated with pars plana vitrectomy with silicone oil tamponade. Ophthalmic Genet 42, 615-618, doi:10.1080/13816810.2021.1925927 (2021).
- Broadhead, G. K., Grigg, J. R., McCluskey, P., Korsakova, M. & Chang, A. A. Bevacizumab for choroidal neovascularisation in enhanced S-cone syndrome. Doc Ophthalmol 133, 139-143, doi:10.1007/s10633-016-9555-9 (2016).
- Bertoli, F., Pignatto, S., Rizzetto, F. & Lanzetta, P. A 5-Year-Old Case of Choroidal Neovascularization in Enhanced S-Cone Syndrome Treated with Ranibizumab. Case Rep Ophthalmol 9, 510-515, doi:10.1159/000495743 (2018).
Faculty Approval by: Paul Bernstein, MD, PhD
Copyright: Copyright Ramshekar and Ronquillo, ©2023. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/
Identifier: Moran_CORE_126913
Lyme Disease-Associated Uveitis: A Case Report and Review Emphasizing the Importance of Travel History and Geographic Considerations
Home / Intraocular Inflammation and Uveitis / Infectious Uveitis
Title: Lyme Disease-Associated Uveitis: A Case Report and Review Emphasizing the Importance of Travel History and Geographic Considerations
Authors: Andrew DesLauriers, BA; Marissa Larochelle, MD
Photographer: Rich Ordonez
Date: 08/09/2023
Keywords/Main Subjects: lyme disease, intermediate uveitis, anterior uveitis, travel history
Diagnosis: Lyme Disease-Associated Intermediate and Anterior Uveitis
Description of Case:
Introduction:
Lyme disease, caused by the Borrelia genus of bacteria transmitted through Ixodes ticks, is primarily reported in the Northeast and Mid-Atlantic regions of the United States, as well as in certain parts of Europe and Japan.1,2 Ocular involvement can occur at any stage of the disease, presenting with diverse manifestations, including uveitis. Early identification of Lyme-associated uveitis is crucial to initiate appropriate treatment and prevent long-term complications. Lyme-associated uveitis should be considered in the differential diagnosis of patients with new-onset uveitis and a history of travel to endemic areas.
Case Presentation:
In early August, a 10-year-old male presented to the Moran Eye Center in Utah with sharp, bilateral eye pain, blurred vision, and increased redness for three days. He reported a history of mild, intermittent eye redness without pain for three months prior to presentation. Additionally, one month before the increase in ocular symptoms, the patient experienced a brief generalized illness with fevers, headache, and cervical/post-cervical and submandibular lymphadenopathy, initially attributed to a self-limited viral illness. The patient, who had recently been diagnosed with autoimmune thyroiditis and a strong family history of autoimmune diseases, reported no previous ocular history. The patient’s mother reported that he regularly interacts with several stray cats near their home, but there were no instances of reported bites or scratches. Additionally, the patient and his family had vacationed in Vermont, a Lyme disease endemic area, three months prior to his presentation at the Moran Eye Center, though no tick bites were reported during their trip.
Examination and Diagnosis:
On examination, the patient had 1-2+ mixed cells in the anterior chamber and 1+ cell and 2+ vitreous haze bilaterally with notable vitreous debris. Fluorescein angiography revealed mild diffuse vascular leakage in both eyes. Based on the clinical picture, the patient was diagnosed with bilateral, simultaneous anterior and intermediate uveitis. Initial laboratory workup was significant for positive Bartonella IgM (1:256) but negative Bartonella IgG. Consequently, the patient was treated for presumed Bartonella infection with doxycycline and rifampin, along with topical prednisolone, cyclopentolate, and an oral prednisone taper to manage inflammation and prevent complications. The patient was referred to Infectious Disease clinic and further history taking revealed hiking in Lyme-endemic Vermont, so Lyme serology was added to the lab work up.
Treatment and Follow-Up:
Two weeks later, additional lab results indicated a positive Lyme ELISA and Immunoblot assay. While the initial Bartonella IgM had been elevated, a repeat Bartonella IgM test was negative (1:64), and two Bartonella IgG assays were also both negative, indicating that the initial positive IgM was likely a false-positive. Fortunately, doxycycline is effective in the treatment of both Bartonella and Lyme Borreliosis, so the patient had already been started on an effective regimen. Rifampin was discontinued, and the patient continued doxycycline for an additional 6 weeks. Following a two-month course of doxycycline with an oral prednisone taper, the patient’s symptoms had completely resolved, and a clinical examination showed no remaining signs of intraocular inflammation. The patient remained symptom-free, with no intraocular inflammation or recurrences at 11 months after the initial presentation.
Lyme Disease Overview:
The Borrelia genus of bacteria, transmitted through a bite from an Ixodes tick, cause Lyme disease, which progresses through three clinical stages. Stage 1 is characterized by a bulls-eye rash (Erythema Migrans) at the infection site in around 80% of patients, accompanied by constitutional flu-like symptoms in some cases. Stage 2 involves hematogenous spread to organs, leading to a variety of sequalae, including meningitis, neuropathies, and acute carditis. Stage 3 presents months to years post-inoculation with chronic manifestations, most commonly oligoarticular arthritis. Notably, 2-3% of Lyme disease patients present with Stage 2 or Stage 3 sequelae within days of exposure.3 Infection with Borrelia tends to peak during the late spring or early summer in endemic areas.3
Ocular Involvement in Lyme Disease:
Ocular involvement, typically bilateral, can occur at any disease stage.4 The most common ocular symptom associated with Lyme disease is a follicular conjunctivitis, occurring in approximately 11% of patients most commonly during Stage 1 of disease.5 Stages 2 and 3 of Lyme disease are associated with a variety of symptoms including all types of uveitis, retinal vasculitis, neuroretinis, episcleritis, keratitis, papillitis, optic neuritis, and cranial nerve palsies of nerves III, V, VI, and VII.4,6
Lyme-Associated Uveitis:
Lyme uveitis, an uncommon manifestation of Stage 2 and Stage 3 Lyme disease, comprises up to 4.3% of all uveitis cases at referral centers in endemic areas; however, the reported prevalence varies widely and is much lower in non-endemic areas.4,7 Patients typically present with symptoms such as eye pain, redness, blurred vision, new floaters, and photophobia. The most common presentation is an intermediate uveitis; however, cases of anterior, posterior, and panuveitis have also been reported.4 Uveitis is commonly accompanied by retinal vasculitis. The uveitis can be granulomatous or non-granulomatous in nature.8 Published reports have described varied clinical findings of Lyme uveitis in different patients, with some demonstrating choroidal neovascularization and others showing multifocal white dots in the posterior pole, resembling white dot syndromes such as acute posterior multifocal placoid pigment epitheliopathy (APMPPE).9,10,11
Diagnosis and Management:
Lyme-associated uveitis should be considered in any patient presenting with new-onset uveitis after travel to a Lyme-endemic area. A detailed history should focus on possible exposure and any symptoms outside of eye-related issues, though ocular involvement can be the sole manifestation of Lyme infection, meaning patients may not have other systemic symptoms.4,6 Particular attention should be paid to patients who report spending any amount of time outdoors in an endemic region, engaging in activities such as hiking, gardening, hunting, or forestry work.3
Tissue biopsies are seldom useful in the detection of ocular Borrelia infection.4 Routine screening for Lyme disease in all uveitis patients isn’t recommended due to the low incidence of Lyme-associated uveitis. However, in the right clinical context and with a history of travel to Lyme-endemic areas, serum antibody testing can be used to confirm the diagnosis. Lyme-associated uveitis management should include regular surveillance, and multi-modal imaging is useful for monitoring progression and treatment response.11
Treatment:
Borrelis burgdorferi, the species of bacteria causing Lyme disease in the United States, is typically sensitive to tetracyclines and many B-lactam antibiotics. Doxycycline, ceftriaxone, and amoxicillin can treat any stage of disease, with ceftriaxone preferred for CNS involvement.3,4 These medications are also effective in treating ocular disease, with some studies suggesting use of a cephalosporin for better ocular penetration.12 Steroid treatment alone does not worsen disease but is insufficient in resolving ocular complications.4 Lyme-associated uveitis typically requires a combined approach of both antibiotic treatment and management of inflammation.
Discussion:
This case illustrates the importance of maintaining a high suspicion for Lyme disease in patients with uveitis if there is a report of recent travel to Lyme-endemic areas. Conversely, it is important to note that Lyme disease is a less likely cause of uveitis in patients without exposure to an endemic region, for example, residents of Utah who have not travelled out of the state. While there are small populations of ticks in Utah that could potentially carry Lyme disease, tests conducted on samples of these ticks have not detected the presence of Borrelia bacteria.13 Even in endemic areas, Lyme disease is an uncommon cause of uveitis, however it should be considered in patients with the appropriate risk factors such as a history of time spent outdoors and additional clinical symptoms. Please see the geographic distributions of reported Lyme disease included in the resources section below to help guide risk stratification based on travel history.
Lyme-associated uveitis can present in various forms, making it crucial to include this infectious etiology in the differential diagnosis when risk factors are present and perform appropriate antibody testing for confirmation. In this case, the patient’s travel to an endemic area in late spring placed him at risk of Lyme exposure. His intermittent eye redness preceding the acute uveitis episode was likely attributable to the follicular conjunctivitis often reported in Lyme disease’s Stage 1. Furthermore, the febrile illness he experienced one month prior to presenting at the Moran Eye Center was likely a systemic manifestation of Lyme disease. Early identification allows for timely treatment and prevents vision-threatening complications.14 Untreated Lyme uveitis, although rare, can result in complete loss of vision and phthisis bulbi.15
Conclusion:
Lyme-associated uveitis, though uncommon, can lead to serious complications. This case report emphasizes the significance of clinical acumen in diagnosing and treating vision-threatening diseases related to Lyme borreliosis. Awareness of Lyme disease’s geographic distribution and risk factors can guide risk stratification based on travel history, helping to identify cases promptly and initiate appropriate management. Clinicians in non-endemic areas should maintain a high index of suspicion for Lyme uveitis in patients with relevant travel history, particularly in the setting of characteristic systemic symptoms.
Images or video:

Figure 1: Lyme Disease Map. Distribution of reported lyme disease cases in the United States in 2021. Each green dot represents a case of Lyme Disease reported to the CDC in 2021. States shaded with light blue are regarded as “high incidence states” by the CDC. States shaded in grey are considered low incidence. Lyme Disease Map acquired from the CDC website: https://www.cdc.gov/lyme/datasurveillance/lyme-disease-maps.html

Figure 2. Fluorescein angiography images of the patient’s right eye that were taken upon presentation. The images captured at 0:35 (top) and 5:24 (bottom) after infusion reveal mild diffuse vascular leakage.
Summary of the Case:
Lyme disease, caused by the Borrelia genus of bacteria and transmitted by Ixodes ticks, can lead to a variety of ocular complications including uveitis. Transmission typically occurs in endemic regions with the appropriate ecological factors to allow for bacterial reproduction and transmission. A 10-year-old male presented with eye pain, redness, and blurred vision after vacationing in a Lyme-endemic region, although he had no reported tick bites. His examination and subsequent tests revealed Lyme-associated uveitis. The importance of early identification and treatment is underscored, as untreated cases can result in severe vision complications. Clinicians in non-endemic regions should maintain vigilance for Lyme uveitis in patients with relevant travel history in order to ensure prompt and effective management.
Format: Case Report, Literature Review
References
- Lyme Disease Map | Lyme Disease | CDC. Accessed August 1, 2023. https://www.cdc.gov/lyme/datasurveillance/lyme-disease-maps.html
- Overview | Johns Hopkins Lyme and Tickborne Diseases Dashboard. Accessed August 1, 2023. https://www.hopkinslymetracker.org/overview/
- Steere AC, Strle F, Wormser GP, et al. Lyme borreliosis. Nature Reviews Disease Primers. 2016;2(1):16090. doi:10.1038/nrdp.2016.90
- Bernard A, Seve P, Abukhashabh A, et al. Lyme-associated uveitis: Clinical spectrum and review of literature. Eur J Ophthalmol. 2020;30(5):874-885. doi:10.1177/1120672119856943
- Steere AC, Bartenhagen NH, Craft JE, et al. The early clinical manifestations of Lyme disease. Ann Intern Med. 1983;99(1):76-82. doi:10.7326/0003-4819-99-1-76
- Lesser RL. Ocular manifestations of Lyme disease. The American Journal of Medicine. 1995;98(4, Supplement 1):60S-62S. doi:10.1016/S0002-9343(99)80045-X
- Mikkilä H, Seppälä I, Leirisalo-Repo M, Immonen I, Karma A. The etiology of uveitis: The role of infections with special reference to Lyme borreliosis. Acta Ophthalmologica Scandinavica. 1997;75(6):716-719. doi:10.1111/j.1600-0420.1997.tb00637.x
- Mikkilä HO, Seppälä IJT, Viljanen MK, Peltomaa MP, Karma A. The expanding clinical spectrum of ocular lyme borreliosis. Ophthalmology. 2000;107(3):581-587. doi:10.1016/S0161-6420(99)00128-1
- Kılıç Müftüoğlu İ, Aydın Akova Y, Gür Güngör S. A Case of Lyme Disease Accompanied by Uveitis and White Dot Syndrome. Turk J Ophthalmol. 2016;46(5):241-243. doi:10.4274/tjo.25991
- Amer R, Brannan S, Forrester JV. Inflammatory choroidal neovascular membrane in presumed ocular Lyme borreliosis. Acta Ophthalmol. 2009;87(3):346-348. doi:10.1111/j.1755-3768.2007.01160.x
- Ferro Desideri L, Rosa R, Forte P, et al. Multimodal imaging for the management of Lyme-associated uveitis: A case report from an Italian tertiary center. European Journal of Ophthalmology. Published online January 29, 2023:11206721231154172. doi:10.1177/11206721231154172
- Lindström BE, Skogman BH, Lindström AK, Tallstedt L, Nilsson K. Borrelia Ocular Infection: A Case Report and a Systematic Review of Published Cases. Ophthalmic Res. 2022;65(2):121-130. doi:10.1159/000521307
- Richardson K, Davis R, Ramirez R. Ticks and Tick-Borne Diseases of Utah. Utah State University Extension and Utah Plant Pest Diagnostic Laboratory; 2023.
- Copeland RAJ. Lyme uveitis. Int Ophthalmol Clin. 1990;30(4):291-293. doi:10.1097/00004397-199030040-00019
- Kauffmann DJ, Wormser GP. Ocular Lyme disease: case report and review of the literature. British Journal of Ophthalmology. 1990;74(6):325-327. doi:10.1136/bjo.74.6.325
Faculty Approval by: Marissa Larochelle, MD
Copyright: Andrew DesLauriers, ©2023. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/
Identifier: Moran_CORE_126899
Iridocorneal Endothelial (ICE) Syndrome
Title: Iridocorneal Endothelial (ICE) Syndrome
Author: Krishna Mallem, Drexel University College of Medicine, MD Class of 2024; . Austin Nakatsuka, MD
Date: July 2023
Keywords/Main Subjects: Iridocorneal endothelial syndrome; ICE; Gonioscopy assisted transluminal trab
- Electron microscopy of corneal endothelium in ICE syndrome.
- Polycoria, corectopia and atrophic iris changes in a patient.
eculotomy; GATT
Introduction:
Iridocorneal endothelial (ICE) syndrome is an unusual disorder of the eye that involves an abnormality of the corneal endothelium. ICE syndrome typically affects middle aged women, and occurs sporadically and unilaterally 1,2. It consists of three clinical variants, which are Chandler syndrome, essential iris atrophy, and iris nevus or Cogan-Reese Syndrome. The distinction between these variants is based on clinical exam findings. Abnormalities of the corneal endothelium in ICE syndrome can lead to varying degrees of corneal edema, iris atrophy, and secondary angle closure glaucoma. This condition can be potentially blinding due to glaucoma recalcitrant to conventional therapies and recurrent corneal edema1-4. We present a case of a patient with ICE syndrome who undergoes gonioscopy assisted transluminal trabeculotomy (GATT) for uncontrolled IOP on medical therapy.
Photos taken from Moran Eye Center archives.
Pathophysiology:
Similar to corneal guttata found in Fuchs endothelial dystrophy, the corneal endothelium in patients with ICE syndrome is described to have a “beaten bronze” appearance. Scanning and tunneling electron microscopy of endothelial cells in patients with ICE syndrome reveal a population of well differentiated epithelial-like cells in place of normal endothelium. This cell population displays migratory characteristics, and is believed to migrate posteriorly onto the trabecular meshwork and the iris. As this tissue contracts within the angle and the iris, peripheral anterior synechiae (PAS) may form, and the iris may undergo morphological changes. Contraction of tissue can also predispose patients to secondary angle closure glaucoma. Corneal edema can develop as a consequence of elevated intraocular pressure as well as due to failure of the normal pump function of the dysfunctional endothelium3-8.
Case presentation:
Our patient is a 51 year old male who presented in February 2017 for glaucoma evaluation in the left eye (OS). IOP on examination was 34. Corneal pachymetry showed a corneal thickness of 523 microns OS. Gonioscopy revealed a broad area of peripheral anterior synechiae (PAS) temporally, with smaller areas of PAS inferiorly. Slit lamp exam was significant for diffuse endothelial guttae-like changes in the cornea with an oval shaped pupil. IOP and slit lamp exam of the right eye were unremarkable. Baseline visual fields were obtained and showed scattered defects in both eyes. Baseline optical coherence tomography (OCT) of the retinal nerve fiber layer (RNFL) revealed normal thickness in both eyes. Given examination findings at the baseline visit, the patient was diagnosed with ICE syndrome and was started on latanoprost once daily OS for intraocular pressure control.
The patient was monitored regularly and over the course of several years his medical therapy was escalated due to persistently high IOPs as well as changes on field and OCT testing. In March 2022, the patient was on maximal medical therapy with netarsudil-latanoprost, dorzolamide-timolol, and brimonidine in the left eye. Despite this, his IOP was 37 on the left. Slit lamp examination at this time showed a distorted pupil with high PAS temporally. Visual field testing showed a subtle superior arcuate scotoma OS. OCT RNFL showed significant thinning inferiorly and superiorly OS. The decision to proceed with surgery was made given the patient’s young age and long term prognosis due to medically uncontrolled IOP.
Patient underwent gonioscopy assisted transluminal trabeculotomy (GATT) with anterior goniosynechiolysis without cataract extraction in May of 2022. After successful surgery without complications, the patient’s iop quickly normalized and was maintained over a year later on two drops. OCT findings 6 months after surgery revealed stability, however, there were signs of progression 1 year following the procedure, despite well controlled IOPs. Additionally, the patient has recently developed corneal guttae and edema which is currently being treated medically with hypertonic . Although the patient’s IOP continues to be well controlled, the current focus is now on controlling corneal edema, with consideration for corneal transplantation in the future if the cornea does not recover with medical therapy alone.
Discussion:
This is a unique case of a patient with ICE syndrome who was managed with GATT and goniosynechiolysis in the left eye for uncontrolled IOP and progressive glaucomatous changes. To our knowledge, there is not another case of GATT or other microinvasive glaucoma surgery (MIGS) being performed in a patient with ICE syndrome in the literature. It is well documented that filtering procedures in ICE syndrome are only modestly successful at 5 years (53% with drainage device and 29% with trabeculectomy)⁸ and often need to be repeated to obtain IOP control. Although GATT has successfully controlled IOP one year out from surgery, there is still evidence of OCT progression and further surgical treatment may be necessary. Furthermore, the patient has developed more clinically significant corneal edema and guttae, suggesting corneal decompensation, which may require surgical intervention with a corneal transplant. This case highlights the difficulty in managing patients with ICE syndrome and documents the novel use of GATT for IOP control in ICE syndrome.
References:
- Laganowski, H. C., Muir, M. G. K., & Hitchings, R. A. (1992). Glaucoma and the iridocorneal endothelial syndrome. Archives of Ophthalmology, 110(3), 346-350.
- Dubey, S., Jain, K., Singh, S., & Mukhejee, S. (2021). Iridocorneal Endothelial Syndrome with Coexisting Macular Edema and Neurosensory Detachment: An Unusual Case Report. Journal of Current Glaucoma Practice, 15(3), 149.
- Campbell, D. G., Shields, M. B., & Smith, T. R. (1978). The corneal endothelium and the spectrum of essential iris atrophy. American journal of ophthalmology, 86(3), 317-324.
- Basic and Clinical Science Course (BCSC). American Academy of Ophthalmology, (2010-2011), 142-144.
- Eagle, R. C., Font, R. L., Yanoff, M., & Fine, B. S. (1979). Proliferative endotheliopathy with iris abnormalities: the iridocorneal endothelial syndrome. Archives of Ophthalmology, 97(11), 2104-2111.
- Doan A, Alward W: Iridocorneal Endothelial Syndrome (ICE) – essential iris atrophy : 63-year-old female with PAS, “iris mass”, corectopia, and increased IOP OS. February 21, 2005; Available from: http://www.EyeRounds.org/cases/case14.htm.
- Levy, S. G., Kirkness, C. M., Moss, J., Ficker, L., & McCartney, A. C. (1996). The histopathology of the iridocorneal-endothelial syndrome. Cornea, 15(1), 46-54.
- Doe, E. A., Budenz, D. L., Gedde, S. J., & Imami, N. R. (2001). Long-term surgical outcomes of patients with glaucoma secondary to the iridocorneal endothelial syndrome. Ophthalmology, 108(10), 1789-1795.
Intraocular Lens (IOL) Opacification and Calcification in Patients with Hydrophilic Lenses
Title: Intraocular Lens (IOL) Opacification and Calcification in Patients with Hydrophilic Lenses
Author (s): Cuneyt Ozkardes, MS; Kevin Eid, MD; Austin Nakatsuka, MD
Date: 7/20/2023
Keywords/Main Subjects: IOL; cataract complications; hydrophilic lens; calcification.
Diagnosis: Calcification of a hydrophilic intraocular lens.
Summary of the Case:
- Intraocular Lens (IOL) opacification is a late post-operative complication, often caused by calcification of the lens material, particularly in hydrophilic lenses.
- This presentation can easily be mistaken for posterior capsule opacification (PCO), therefore, it is important to conduct a thorough ocular history and exam, especially in eyes with hydrophilic IOLs.
- The only treatment option currently for this condition is lens exchange surgery.
Description of Case:
Introduction
Intraocular Lens (IOL) opacification is a late post-operative complication of cataract surgery, especially in patients with hydrophilic lenses.1 The most common cause of opacification is calcification of the lens material.2 Proposed causes of this phenomenon include reactions with post-operative intracameral substances (i.e. Silicone, gas, viscoelastic), metabolic changes in the anterior chamber, or inflammatory reactions caused by surgical procedures.3-5 The only known treatment for this phenomenon is explantation with or without exchanging of the lens.6,7 In addition to their association with lens calcification, meta-analyses have shown hydrophilic lenses tend to have higher PCO rates compared to lenses of other materials.8 Because of this known complication associated with hydrophilic lens material, the most common implanted lenses are currently made of hydrophobic material.
Case Presentation
An 83-year-old male patient with a known history of pseudoexfoliation glaucoma in both eyes presented to our clinic with complaints of slowly worsening blurry and limited vision in the right eye over the past six months. Despite these symptoms, previous slit lamp examinations during this period had been unremarkable with BCVA of 20/20 bilaterally. The patient had undergone trabeculectomy in the right eye 21 months prior, which was complicated by a choroidal hemorrhage and subsequent choroidal detachment one week later. He was treated conservatively with prednisolone and atropine drops daily, as well as oral prednisone. His visual acuity improved from 20/300 at presentation to 20/20 after 8 weeks of treatment.
Upon examination during the current visit, BCVA in the right eye was 20/20. Slit-lamp examination revealed a central cloudy opacity in the posterior chamber intraocular lens (PCIOL), with haptics positioned at 2 and 8 o’clock. The left eye showed no signs of opacification or other complications. Based on the clinical findings and the significant impact on visual function, the decision was made to proceed with an IOL exchange surgery to address the opacification using a hydrophobic TECNIS Eyhance IOL.
The original IOL, placed nearly 13 years prior, was removed and sent for pathological analysis. It was identified as an Akreos Bausch and Lomb one-piece [plate] hydrophilic acrylic posterior capsule IOL (Model MI60L). The pathology report described the specimen as having a deposition of a white granular material on the anterior surface of the IOL in the center of the optic. The deposition was consistent with calcium and was specifically deposited centrally, denoting the area where the anterior capsulotomy is open. The peripheral part of the optic as well as the footplates showed no deposition of this material.
Follow-up examination eleven weeks after the IOL exchange surgery revealed a well-centered IOL with mild posterior capsule opacification (PCO). The patient’s BCVA was 20/20, with the patient noting he was much happier with his vision and seeing well. He expressed overall satisfaction with the new lens and reported no further visual complaints. Continued monitoring and regular follow-up visits were scheduled to assess the long-term stability of the IOL and to manage any potential future complications.
Images or video:

Figure 1. Slit-lamp examination revealing central cloudy opacification of the intraocular lens (IOL ).

Figure 4. Enhanced view revealing widespread calcification (seen in the image as diffuse round globules ) coating the central and anterior surfaces of the extracted IOL.
Format: Case Report
References:
- Grzybowski, A., Markeviciute, A., & Zemaitiene, R. (2020). A narrative review of intraocular lens opacifications: Update 2020. Annals of Translational Medicine, 8(22).
- Drimtzias, E. G., Rokidi, S. G., Gartaganis, S. P., & Koutsoukos, P. G. (2011). Experimental investigation on mechanism of hydrophilic acrylic intraocular lens calcification. American Journal of Ophthalmology, 152, 824-833.
- Werner, L., Wilbanks, G., Nieuwendaal, C. P., et al. (2015). Localized opacification of hydrophilic acrylic intraocular lenses after procedures using intracameral injection of air or gas. Journal of Cataract and Refractive Surgery, 41, 199-207.
- Stanojcic, N., Hull, C., & O’Brart, D. P. (2020). Clinical and material degradations of intraocular lenses: A review. European Journal of Ophthalmology, 30, 823-839.
- Pérez-Vives, C. (2018). Biomaterial Influence on Intraocular Lens Performance: An Overview. Journal of Ophthalmology, 2018, 2687385.
- Haymore, J., Zaidman, G., Werner, L., et al. (2007). Misdiagnosis of hydrophilic acrylic intraocular lens optic opacification: Report of 8 cases with the MemoryLens. Ophthalmology, 114, 1689-1695.
- Werner, L. (2007). Causes of intraocular lens opacification or discoloration. Journal of Cataract and Refractive Surgery, 33, 713-726.
- Findl, O., Buehl, W., Bauer, P., & Sycha, T. (2010). Interventions for preventing posterior capsule opacification. Cochrane Database of Systematic Reviews, 2. CD003738.
Faculty Approval by: Austin Nakatsuka, MD
Identifier: Moran_CORE_126859
Copyright Cuneyt Ozkardes, ©2023. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/
Advancing Wavelike Epitheliopathy
Home / External Disease and Cornea / Clinical Approach to Ocular Surface Disorders
Title: Advancing Wavelike Epitheliopathy: A subtype of partial limbal stem cell deficiency
Author (s): William B. West Jr.
Photographer: Photos courtesy of Dr. Majid Moshirfar
Date: 9/3/20
Keywords/Main Subjects: Advancing Wavelike Epitheliopathy, Partial Limbal Stem Cell Deficiency, Limbal Stem Cell Deficiency, Epitheliopathy
CORE Category:
External Disease and Cornea > Clinical Approach to Ocular Surface Disorders > Limbal Stem Cell Deficiency > Advancing Wavelike Epitheliopathy
Diagnosis: Advancing Wavelike Epitheliopathy
Description of Image:
Advancing Wavelike Epitheliopathy (AWE) is a form of ocular surface disorder that was first described by D’Aversa et. al. in 1997. It is characterized by a well-defined epithelial plaque with a rough, wavelike appearance and punctate pattern on fluorescein staining. A sub-epithelial haze may also be present. The plaque arises from the corneal limbus, most often superiorly, and expands toward the visual axis. Patients present with a history of progressive vision loss over a period of several months, as well as ocular irritation and foreign body sensation.
While the exact pathophysiology is poorly understood, AWE is presumed to be a subtype of partial limbal stem cell deficiency (PLSCD). The limbal stem cells are the progenitors of the corneal epithelium and reside at the limbus. Epithelial cells migrate from the limbus toward the center of the cornea, forming the corneal surface. In a limbal stem cell deficiency, some or all of the limbal stem cells become dysfunctional and fail to produce normal epithelium. This process most commonly results in breakdown of the epithelial layer causing surface inflammation, which in turn causes neovascularization or conjunctival invasion of the cornea.
In contrast, in AWE the epithelial surface becomes abnormal but does not break down and conjunctivalization does not usually occur. AWE has been associated with a history of ocular trauma, surgery, or chemical or toxic exposure to the ocular surface.
While the potential differential diagnosis for this disorder is broad, likely considerations include:
- Epithelial ingrowth
- Dry eye disease
- Diffuse Lamellar Keratitis (DLK)
- Central Toxic Keratopathy (CTK)
- Limbal Stem Cell Deficiency (LSCD)
- Ocular Surface Squamous Neoplasia
- Conjunctival Intraepithelial Neoplasia
- Herpes Keratitis
Initial treatment for this disease incudes conservative measures to reduce inflammation and maximize healing. These treatments include artificial tears, oral doxycycline, or topical corticosteroids. Superficial keratectomy can be used, and usually provides temporary resolution of the plaque; however, the plaque nearly always recurs. Adding topical silver nitrate, applied via cotton swab to the affected area after corneal debridement, appears to produce stable recovery. Simple limbal stem cell transplant can be performed to regenerate the corneal limbus, if silver nitrate is unsuccessful. This is usually performed by harvesting limbal stem cells from the unaffected eye (if the disease is not bilateral). Interferon alpha-2b, topical or oral cyclosporine, punctal plugs, scleral lenses, vitamin A, autologous blood serum, amniotic membrane drops, and fluorometholone may be helpful in treating AWE, as they have been used successfuly in treating other varieties of PLSCD. Topical corticosteroids have not been shown to be effective.
This video shows the left eye of a 36-year-old male with a six-month history of vision loss and foreign body sensation after LASIK. Before surgery, he had a history of chronic redness and irritation in the left eye before surgery, as well as a possible chemical injury to that eye as a child. The classic wavelike plaque can be seen advancing from the limbus both inferiorly and superiorly.
Conclusion:
Advancing Wavelike Epitheliopathy is a type of partial limbal stem cell deficiency forming a characteristic wavy epithelial plaque that expands from the limbus toward the visual axis. It is associated with injury to the limbal stem cells and is treated with superficial keratectomy and silver nitrate or limbal stem cell transplant. Prognosis is typically excellent after treatment.
References:
- D’Aversa G, Luchs JL, Fox MJ, Rosenbaum PS, Udell IJ. Advancing wave-like epitheliopathy: Clinical features and treatment. Ophthalmology [Internet]. American Academy of Ophthalmology, Inc; 1997;104(6):962–969. Available from: http://dx.doi.org/10.1016/S0161-6420(97)30199-7 PMID: 9186437
- Rossen J, Amram A, Milani B, et al. Contact Lens-induced Limbal Stem Cell Deficiency. Ocul Surf. 2016;14(4):419-434. doi:10.1016/j.jtos.2016.06.003
- Kim BY, Riaz KM, Bakhtiari P, et al. Medically Reversible Limbal Stem Cell Disease: Clinical Features and Management Strategies. Ophthalmology. 2014;121(10):2053-2058. doi:10.1016/j.ophtha.2014.04.025
- Moshirfar M, Hastings JP. Unilateral progressive epitheliopathy after LASIK [Internet]. Journal of Cataract and Refractive Surgery. Lippincott Williams and Wilkins; 2020 [cited 2020 Aug 25]. p. 646–651. Available from: https://pubmed.ncbi.nlm.nih.gov/32271301/ PMID: 32271301
- Tan JCK, Tat LT, Coroneo MT. Treatment of partial limbal stem cell deficiency with topical interferon α-2b and retinoic acid. Br J Ophthalmol. 2016;100(7):944-948. doi:10.1136/bjophthalmol-2015-307411
- Majid Moshirfar MD., William B. West jr., Yasmyne C. Ronquillo. Advancing Wavelike Epitheliopathy. Statpearls. 2020. https://pubmed.ncbi.nlm.nih.gov/32119296/
- William B. West jr., Yasmyne C. Ronquillo, Majid Moshirfar MD. Advancing Wavelike Epitheliopathy. Eyewiki. 2020.
- https://eyewiki.aao.org/Advancing_Wavelike_Epitheliopathy#:~:text=Advancing%20Wavelike%20Epitheliopathy%20is%20an,the%20center%20of%20the%20cornea.
Faculty Approval by: Griffin Jardine, MD
Footer:
- Copyright statement: Copyright William B. West Jr., ©2020. For further information regarding the rights to this collection, please visit: URL to copyright information page on Moran CORE
- Identifier: Moran_CORE_29777
Disclosure (Financial or other): Nothing to disclose.
Custom Implant for Correction of Enophthalmos After Orbital Fracture Repair
Home / Orbit, Eyelids, and Lacrimal System / The Anophthalmic Socket
Title: Custom Implant for Correction of Enophthalmos After Orbital Fracture Repair
Author: Benjamin West, MSIV, Loma Linda University
Date: 7/24/2018
Image or video:

Figure 1. CT scan at admission demonstrating right medial wall blow-out fracture as well as extensive damage to the right globe.

Figure 2. CT scan at 5 months after enucleation and initial fracture repair showing significant right sided enophthalmos and persistence of medial orbital wall fracture.
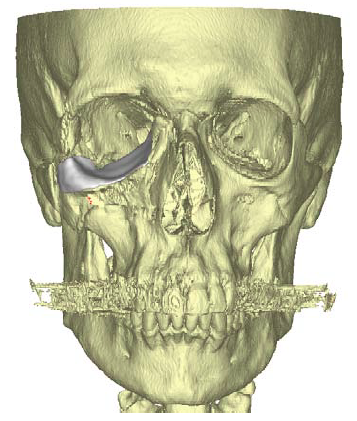
Figure 3. 3D virtual reconstruction of patient anatomy with custom porous polyethylene implant in place.
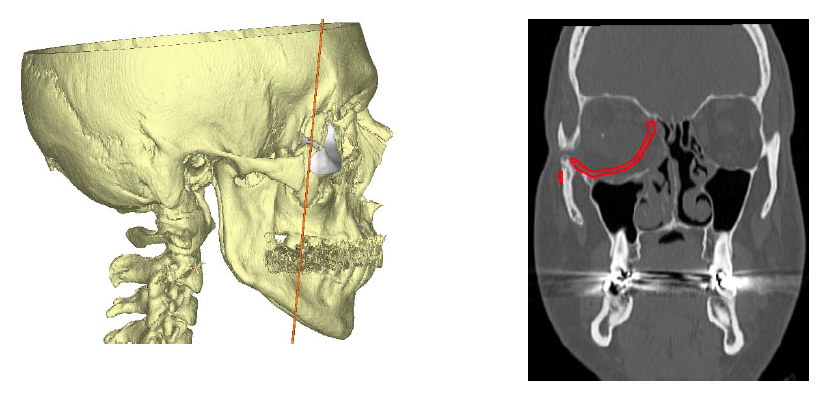
Figure 4. CT scan showing proposed position of custom porous polyethylene implant and subsequent reduction of orbital volume to correct right-sided enophthalmos.
Keywords/Main Subjects: Orbital fractures, Le Fort fractures, Open Globe, Enophthalmos, Orbital Implant; Porous Polyethylene; Custom Implant
CORE Category: Orbit, Eyelids and Lacrimal System > The Anophthalmic Socket > 4. Orbital Implants > “Custom Implant for Correction of Enophthalmos After Orbital Fracture Repair: Case Report”
Diagnosis: Enophthalmos after orbital fracture repair
Description of Image:
This is a 40 year old male who presented to the emergency department after being struck by a heavy chain in the face at work. Initial examination showed extensive facial lacerations (brow, nose, eyelid and temple) as well as a 1 cm laceration of the right cornea and sclera with expulsion of orbital contents. CT scans at admission showed hemi-Le Fort fractures 1, 2 and 3 on the right side, with a zygomaticomaxillary complex fracture and fracture of all four orbital walls (Figure 1). The left side exhibited a hemi-Le Fort 2 fracture, as well as medial and inferior orbital wall fractures.
Due to the extensive damage to the globe, the patient was subsequently taken to the operating room for enucleation and implantation of an 18 mm porous polyethylene implant by oculoplastics. Plastic surgery completed the facial fracture repair. Floating zygoma fractures were plated and anchored to the frontal bone and the right orbital floor was plated with resorbable material to contain the orbital implant in normal position.
At 5 months post-op the patient was noted to have significant right-sided enophthalmos > 2 mm, as well as a severely sunken superior sulcus. Repeat imaging showed osseous bridging of the majority of facial fractures, but persistent right orbit medial blowout fracture with medial herniation of orbital contents and irregularity of the right orbital floor (Figure 2). At this time the patient was agreeable to undertake enophthalmos repair of the right eye with implantation of a customized porous polyethylene implant.
Fine-cut updated CT images were sent to Stryker where a virtual reconstruction plan was made according to the imaging and surgeon specifications. The orbital implant was made from porous polyethylene using a 3D printer and tailored specifically to the anatomy of the patient (Figures 3 and 4).
The patient was taken to the operating room with oculoplastics where an incision was made in the inferior fornix of the right lower eyelid. Dissection was carried out to the inferior orbital rim with subsequent elevation of the periosteum and periorbita. The custom implant was then inserted into the orbit and positioned to correct the enophthalmos as compared to the left eye. The implant was screwed into place at the inferior orbital rim.
At the following post-op examination significant improvement was noted in the enophthalmos and sunken superior sulcus of the right eye with high patient satisfaction. Mild ptosis was noted of the right eye and the patient was counseled on possible future repair if unimproved.
Faculty Approval by: Doug Marx
Footer:
- Copyright Moran Eye Center, ©2018. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/
Disclosure (Financial or other):
None
Peripheral Leakage, Avascularity, and Non-perfusion –A Case of Familial Exudative Vitreoretinopathy
Home / Retina and Vitreous / Congenital and Developmental Abnormalities
Title: Peripheral Leakage, Avascularity, and Non-perfusion – A Case of Familial Exudative Vitreoretinopathy
Author (s): Blake H. Fortes, MSIV, Florida International University Herbert Wertheim College of Medicine
Photographer: Moran Eye Center
Date: 6/27/2018
Image or video:

Image 1: Montage color fundus photograph of the right eye demonstrating 1) a vitreous adhesion to the optic nerve with temporal macular traction, 2) vascular dragging and tortuosity, 3) far peripheral fibrotic changes overlying atrophic and pigmentary changes, and 4) exudates in the temporal periphery.
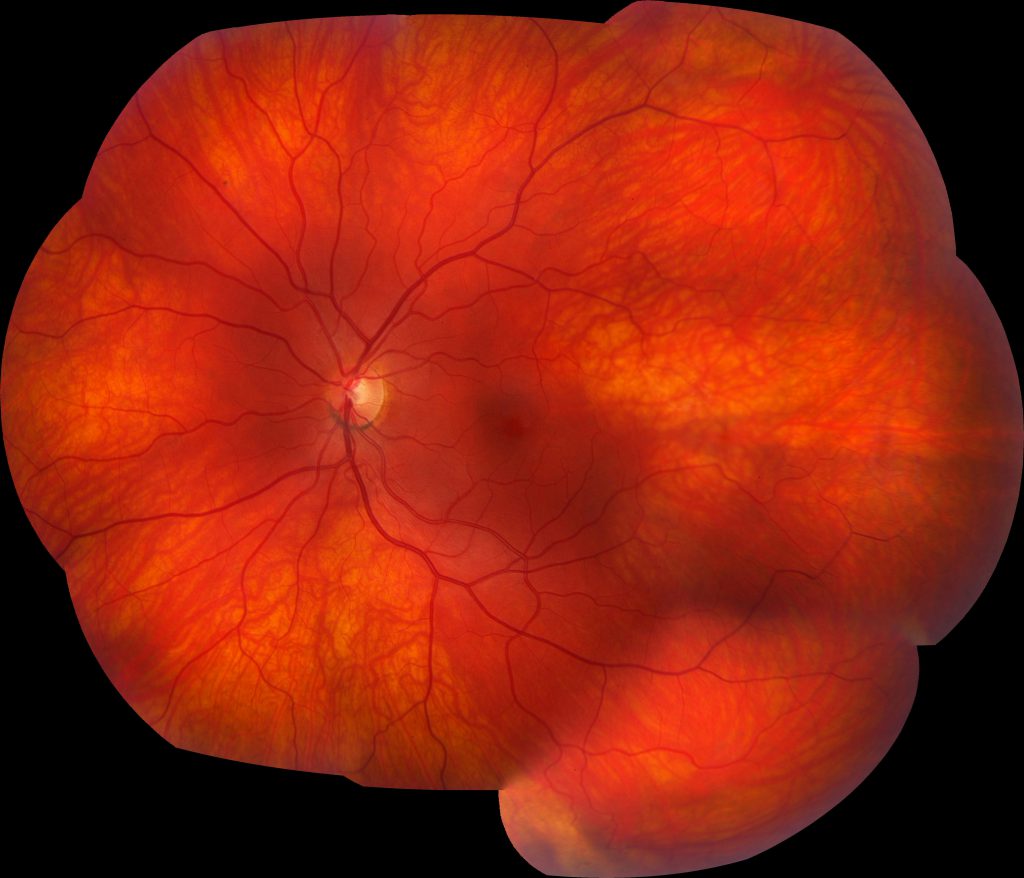
Image 2: Montage color fundus photograph of the left eye demonstrates a relatively normal fundus with some slight vascular tortuosity in the temporal periphery.
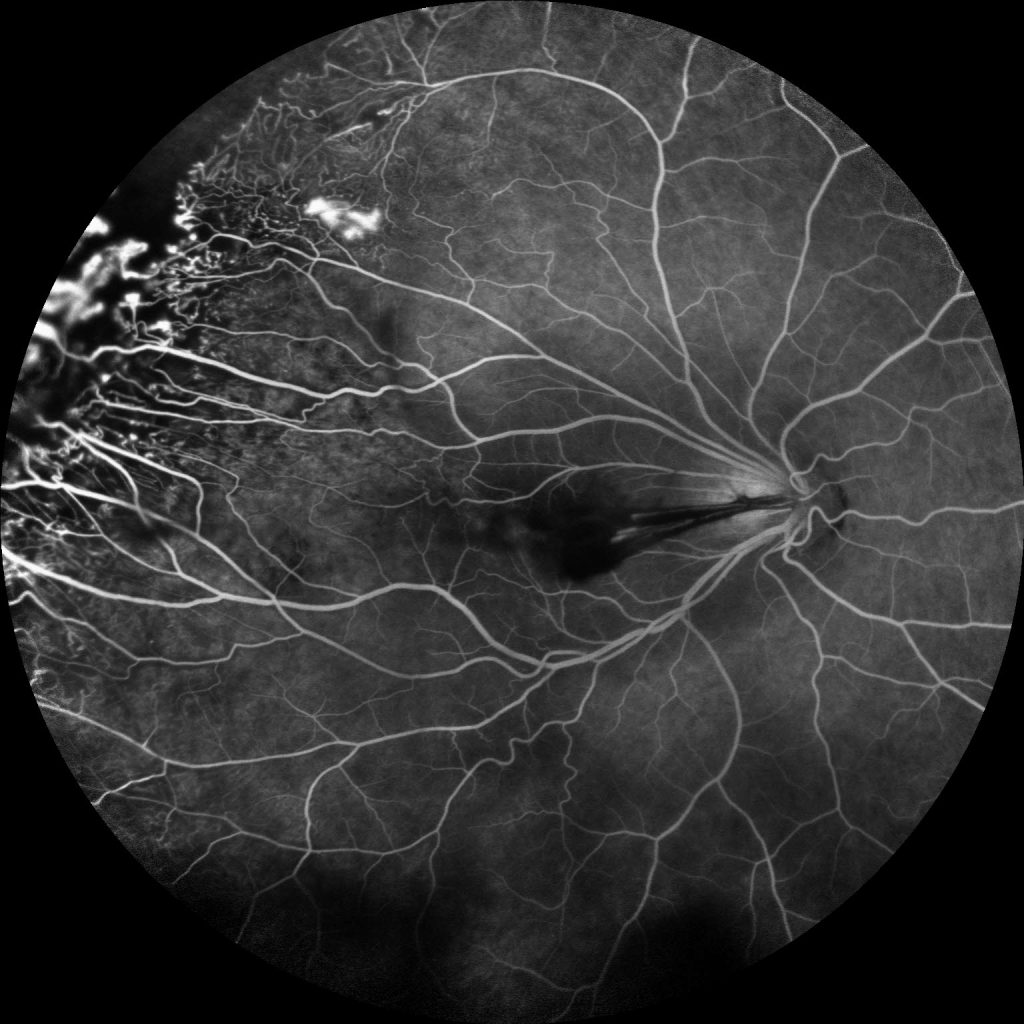
Image 3: Fluorescein angiogram of the right eye demonstrates multiple peripheral areas of focal hyperfluorescence that were shown to increase in intensity in the late phase along with diffuse leakage in the periphery and temporal peripheral non-perfusion.

Image 4: Fluorescein angiogram of the left eye revealing multiple areas of temporal vascular leakage with a broad temporal area of non-perfusion, which illustrates, not only, the importance of wide-field fluorescein angiography for diagnosing familial exudative vitreoretinopathy, but also the disease asymmetry that is characteristic of FEVR.
Keywords/Main Subjects: Familial exudative vitreoretinopathy, FEVR, peripheral avascularity, leakage, non-perfusion, neovascularization
Secondary CORE Category: Pediatric Ophthalmology and Strabismus / Disorders of the Retina and Vitreous
Diagnosis: Familial Exudative Vitreoretinopathy
Summary of Case: Patient is a 21 year old female with a diagnosis of a vasoproliferative tumor in the right eye who noted sudden onset of painless drastic decreased visual acuity in the right eye, which had drastically worsened over the last two months and was accompanied by floaters. She denied any photopsias. She has a history of myopia, and has always noticed decreased visual acuity in the right eye. She has no history of eye trauma, or surgery and was born at term, has a normal developmental history, and denied supplemental oxygen use at birth. Family ocular history was significant for a grandmother who had a retinal detachment requiring multiple surgeries. On exam, her visual acuity with correction in the right eye was 20/125 and in the left eye was 20/30 and was noted to have exotropia of the right eye. Her dilated fundus exam in the right eye revealed a tilted, small optic nerve with a vitreal adhesion from the disc to a temporal scar along with macular edema, temporal macular traction, epiretinal membrane, vascular dragging and tortuosity, as well as a fibrotic white lesion at 10 o’clock, surrounded by retinal pigment epithelial changes, and nearby exudates.
Familial Exudative Vitreoretinopathy:
FEVR is a disorder characterized by incomplete vascularization of the peripheral retina typically due to mutations in the Wnt signaling pathway, which is involved in organogenesis and angiogenesis of the eye. These gene mutations include NDP, FZD4, LRP5, and TSPAN12. Novel mutations in ZNF408 and KIF11 have recently been elucidated, but are not involved in the Wnt signaling pathway. The inheritance pattern varies depending on the mutation and may range from autosomal dominant (most commonly), to autosomal recessive, to X-linked recessive or even sporadic, as only 20-40% of patients with FEVR have a positive family history. Therefore, a negative family history does not exclude this diagnosis. This condition is characterized by variable expressivity and asymmetric disease.
The hallmark and most common finding of FEVR is avascularity in the temporal periphery of the retina with associated retinal neovascularization and fibrosis at the junction between the vascular and avascular retina. This fibrosis may result in traction of the macula and retinal vessels, resulting in macular dragging and radial retinal folds. Macular dragging may result in exotropia, as illustrated in this patient. Subretinal exudation, and any type of retinal detachment (rhegmatogenous, tractional, and exudative) may occur as well. Other less common findings associated with this disorder include secondary epiretinal membrane formation, vitreous hemorrhage, secondary glaucoma (neovascular or phacomorphic), retained hyaloid vascular remnants, and persistent fetal vasculature.
Differential diagnosis includes retinopathy of prematurity, Coats’ disease, Norrie’s disease, osteoporosis pseudoglioma syndrome, incontinentia pigmenti, persistent fetal vasculature, vasoproliferative tumor, and ocular toxocariasis.
The staging for FEVR includes:
- Stage 1: avascular periphery
- Stage 2: retinal neovascularization without exudate (A) or with exudate (B)
- Stage 3: extramacular retinal detachment without exudate (A) or with exudate (B)
- Stage 4: subtotal macula-involving retinal detachment without exudate (A) or with exudate (B)
- Stage 5: total retinal detachment
Only patients who have progressed significantly or are at high risk of progression should be treated. In stage 1-2A disease, the avascular retina should be treated with laser photocoagulation to decrease complications related to retinal neovascularization. Retinal detachment should be treated surgically via pars plana vitrectomy, scleral buckle, or a combination of these two approaches. Retinal exudation and neovascularization may also be managed adjunctively via intravitreal anti-VEGF injection prior to surgery. Due to the unpredictable course of FEVR, lifelong monitoring is indicated. Examination of family members is also warranted to reveal previously undiagnosed cases of FEVR.
Format: Case Presentation
References:
- Chen K, Wang N, Wu W. Familial Exudative Vitreoretinopathy. JAMA Ophthalmol. 2017;135(4):e165487. doi:10.1001/jamaophthalmol.2016.5487.
- Gilmour DF. Familial exudative vitreoretinopathy and related retinopathies. Eye. 2015;29(1):1-14. doi:10.1038/eye.2014.70.
- Natung T, Venkatesh P, Thangkhiew L, Syiem J. Asymmetric presentations of familial exudative vitreoretinopathy. Oman Journal of Ophthalmology. 2013;6(2):129-130. doi:10.4103/0974-620X.116661.
- Ranchod TM, Ho LY, Drenser KA, Capone A, and Trese MT. Clinical presentation of familial exudative vitreoretinopathy. Ophthalmology. 2011;118(10):2070-2075.
- Shastry, B. S. (2009), Persistent hyperplastic primary vitreous: congenital malformation of the eye. Clinical & Experimental Ophthalmology, 37: 884-890. doi:10.1111/j.1442-9071.2009.02150.x
- Shields CL, Kaliki S, Al-Dahmash S, et al. Retinal Vasoproliferative TumorsComparative Clinical Features of Primary vs Secondary Tumors in 334 Cases. JAMA Ophthalmol. 2013;131(3):328–334. doi:10.1001/2013.jamaophthalmol.524
- Sızmaz S, Yonekawa Y, T. Trese M. Familial Exudative Vitreoretinopathy. Turkish Journal of Ophthalmology. 2015;45(4):164-168. doi:10.4274/tjo.67699.
- Tauqeer Z, Yonekawa Y. Familial exudative vitreoretinopathy: Pathophysiology, diagnosis, and management. Asia Pac J Ophthalmol (Phila). 2018;7(3):176-182.
Faculty Approval by: Dr. Albert Vitale
Footer:
- Copyright statement: Copyright Author Name, ©2016. For further information regarding the rights to this collection, please visit: URL to copyright information page on Moran CORE
- Attribution/citation suggestions
Disclosure (Financial or other): None
Hydrogel Intraocular Lens Opacification and Calcification Pathology using a MemoryLens Model
Home / Lens and Cataract / Complications of Cataract Surgery
Title: Hydrogel Intraocular Lens Opacification and Calcification Pathology using a MemoryLens Model
Author(s): Jed H Assam, M.S., and Nick Mamalis, MD
Photographer: Jed H Assam
Date: 7/13/2016
Location in Core: Lens and Cataract > Complications of Cataract Surgery > Complications of IOL Implantation
Keywords / Main Subjects: IOL Calcification, IOL Opacification, MemoryLens, Hydrogels, Hydrophilic Acrylic
Diagnosis / Differential Diagnosis: Posterior Capsular Opacity, Soemmering’s Ring, Anterior Capsule Contraction Syndrome (ACCS)/Capsular Phimosis, Anterior Vitreous Floaters

Figure 1. The anterior surface of an explanted 3-piece hydrophilic acrylic IOL (MemoryLens) with significant calcification shown using light microscopic (large) and stereotactic (small) imaging.
Background
Intraocular lens (IOL) opacification and calcification represent uncommon, but noteworthy causes of blurry vision and decreased visual acuity in pseudophakic patients. Awareness of this pathology becomes particularly important when considering the consequences of reflexively performing initial, errant procedures (nd:YAG and vitrectomy) directed at more common anatomic sources of visual disturbance in pseudophakic populations that typically includes the capsular bag or hyaloid.1,3 A survey (n = 142) evaluating foldable IOL complications requiring removal or secondary interventions identified IOL opacification as a minor cause of postoperative complication in most lens categories evaluated.6 However, for hydrogel (hydrophilic acrylic) IOLs, which represented 4% of the IOLs used in the study, post-operative opacification/calcification was the most common reason for lens removal.6
An explanted, calcified, posterior chamber IOL, MemoryLens (Ciba Vision Corp., Duluth, GA, USA), has been demonstrated in Figure 1. The MemoryLens is a 3-piece foldable hydrogel that was initially released in 1994.3,4 It has been the most heavily documented IOL with postoperative calcification complications in the United States.6 Several other hydrophilic acrylic lenses have also been implicated in calcific opacification as well (Hydroview, Bausch & Lomb; AquaSense, Ophthalmic Innovations International; SC60B-OUV, Medical Development Research).4,7
Pathophysiology:
The time required from initial lens placement to the development of visually significant opacification in hydrogel lenses can take several years.1,7 The mean interval for the MemoryLens IOL was identified by one study examining 106 explanted lenses to be 25.8 ±11.9 months with a range from approximately 3 months to 6 ½ years.1
MemoryLens predisposition to opacification was believed to be related to the buffering process of the lenses manufactured through the year 1999.1,3,4 The mechanism by which granular calcific opacification (Figure 2) occurs in vivo remains unknown. It is presently believed to be a multifactorial event related to the surface ionization of hydrogel under physiologic pH levels which facilitate calcium precipitation.4,7
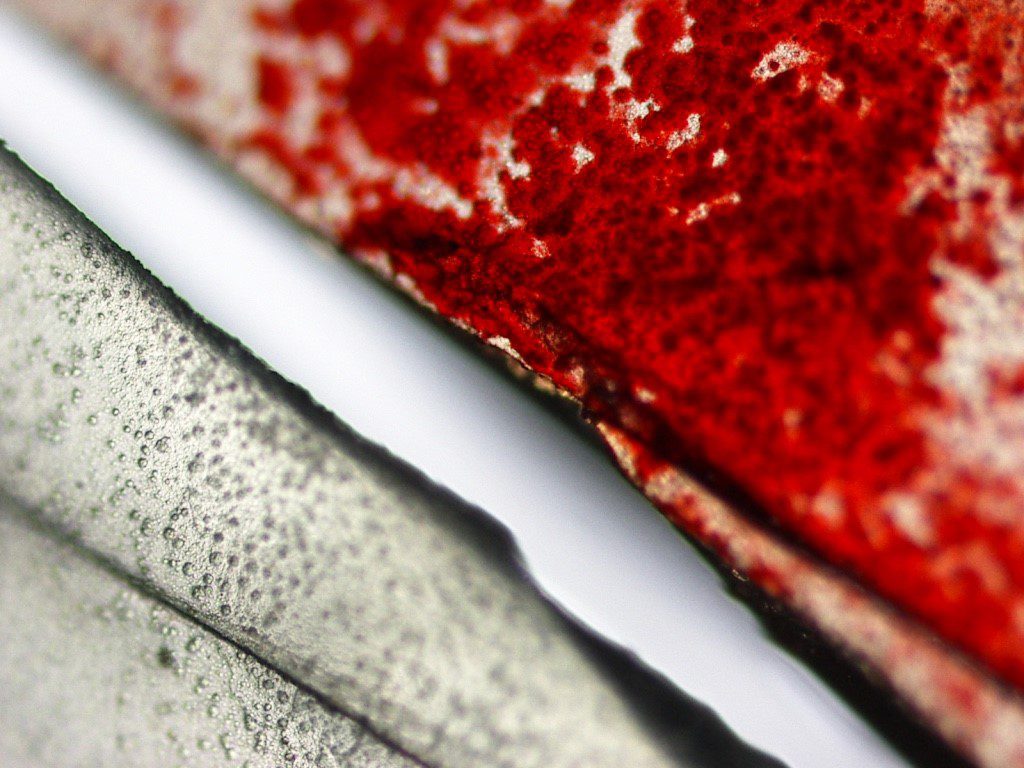
Figure 2. High magnification light microscope image demonstrating Alizeran red staining on half of the calcified MemoryLens optic surface compared to an unstained half with granular deposits of calcium.
Risk Factors/Symptoms:
Some of the risk factors that have been associated with hydrogel IOL calcifications include exposure to surgically introduced exogenous substances such as gas, air, tissue plasminogen activator, and silicone oil. Other risk factors include contact with lens packaging materials and lens polishing techniques.1,8 It is currently unknown whether the direct contact of surgical exogenous substances to the optical surface facilitates calcium precipitation or if such sequela is a consequence of increased inflammation resulting from surgical manipulation.7 Progressive visual loss is the most common primary symptom complaint identified in patients with calcified IOLs.6,7
Diagnosis:
Diagnostically, the presence of calcium may be confirmed on pathologic analysis post-explantation by observing characteristic histochemical staining of granules with Alizeran (1,2-dihydroxyanthraquinone) red, as shown in Figure 2 and Figure 3c, and by electron microscopy coupled with energy dispersive x-ray spectroscopy.8 Diffuse granular deposition is typically noted over the lens body, but tends to be more heavily concentrated on the optic center. In the MemoryLens the coated anterior surface shows heavier calcification than the posterior surface which shows less. Early on the posterior surface typically remains free of deposits (Figure 2b and d).3,4 For hydrogel lenses in general, calcium deposition distribution may be superficial, intralenticular, or both.7

Figure 3. Stereotactic images of a calcified MemoryLens following explantation. Lens opacification from anterior views can be appreciated on both unstained (a) and stained (c) lenses with significant granular calcium deposits. A relatively smooth posterior lens surface without deposition is appreciated on views of unstained (b) and stained (d) lens surfaces.
Treatment:
The only treatment currently available for resolving situations of an opacified calcific IOL includes explantation.5
References:
- Werner L. Causes of intraocular lens opacification or discoloration. Cataract Refract Surg. 2007;33:713-726
- Werner L. Biocompatability of intraocular lens materials. Current Opinion in Ophthalmology. 2008;19:41-49
- Haymore J, Zaidman G, Werner L, Mamalis N, Hamilton S, Cook J, Gillette T. Misdiagnosis of hydrophilic acrylic intraocular lens optic opacification: Report of 8 cases with the MemoryLens. Ophthalmology. 2007;114(9):1689-1695
- Neuhann IM, Werner L, Izak AM, Pandey SK, Kleinmann G, Mamalis N, Neuhann TF, Apple DJ. Late postoperative opacification of a hydrophilic acrylic (hydrogel) intraocular lens. Ophthalmology. 2004;111:2094-2101
- Werner L. Calcification of hydrophilic acrylic intraocular lenses. Am J. Ophthalmol. 2008;146(3):341-343
- Mamalis N, Brubaker J, Davis D, Espandar L, Werner L. Complications of foldable intraocular lenses requiring explantation or secondary intervention—2007 survey update. J Cataract Refract Surg. 2008;34:1584-1591
- Gartaganis SP, Prahs P, Lazari ED, Gartaganis PS, Helbig H, Koutsoukos PG. Calcification of hydrophilic acrylic intraocular lenses with a hydrophobic surface: laboratory analysis of 6 cases. Am J Ophthalmol. 2016;168:68-77
- Werner L, Wilbanks G, Ollerton A, Michelson J. Localized calcification of hydrophilic acrylic intraocular lenses in association with intracameral injection of gas. J Cataract Refract Surg. 2012;38:720-721
Crocodile Shagreen corneal dystrophy
Home / External Disease and Cornea / Corneal Dystrophies and Ectasias
Title: Crocodile Shagreen corneal dystrophy
Author (s): Tanner Ferguson, MSIV, University of South Dakota Sanford School of Medicine, Jeff Pettey, MD, Moran Eye Center, University of Utah
Photographer: James Gilman
Date: 07/31/17
Keywords/Main Subjects: Cornea, corneal mosaic dystrophy, crocodile shagreen
Diagnosis: Crocodile shagreen corneal degeneration
Images:
Image 1: On this anterior view of the cornea, the polygonal pattern of opacities with well demarcated intervening clear spaces is visualized.
Image 2: This photo enables the viewer to appreciate the resemblance to crocodile skin and the distinct appearance of the degenerative disorder.
Image 3: In this photo, the intervening clear spaces amongst the opacities are well visualized and the “scaly” appearance is appreciated. Furthermore, the image permits the viewer to appreciate that it likely involves the posterior portion of the corneal stroma.
Summary of the Case:
A 67 year-old female with past medical history significant for Type II diabetes mellitus presented with blurry vision of 6 months onset that is worse at distance. She also complained of glare at night and difficulty with oncoming headlights while driving. Her BCVA is 20/50 in her right eye and 20/60 in her left eye; her BAT is 20/70 and 20/80 in her right and left eye. On exam, her cataracts were graded as 2+ NS (nuclear sclerotic) and 2+ cortical spoking OU. Her cornea also demonstrated a polygonal pattern of opacities in the posterior stroma with clear intervening spaces, resembling a “crocodile skin.” The clinician did not feel her visual complaints were related to the corneal findings revealed on exam and the findings were documented as crocodile shagreen.
Crocodile shagreen background
Crocodile shagreen is a clinical finding that was initially described in the 1920’s and named by Vogt in 1930.1 The disorder is characterized by a grayish, polygonal pattern of opacities with intervening clear zones across the central cornea that resembles crocodile skin.1,2 Although it is classically found in the central visual axis in the cornea, patients are often asymptomatic. It is a benign, degenerative disorder and is commonly found in the elderly population.3
The pathogenesis of the finding remains unknown. It is typically found in the posterior two-thirds of the corneal stroma. Studies with histopathology have reported the presence of clusters of vacuoles and a sawtooth-like configuration of the lamellar collagen in the corneal stroma3-5. Krachmer et al.5 proposed that this irregular collagenous arrangement in the posterior stroma observed on transmission electron microscopy is thought to contribute to the clinical appearance of the finding under the slit lamp. Furthermore, this report suggested that vision is unaffected because the anterior corneal surface is regular. Although the pathogenesis remains unclear, studies have suggested that the presence of vacuoles amongst degenerating keratinocytes is evidence of a degenerative process.2
Central cloudy dystrophy of François (CCDF) is a disease entity with a similar clinical appearance. However, CCDF is distinguished from crocodile shagreen by its autosomal dominant inheritance pattern and may be seen in younger patients.6 The diagnosis of CCDF may be more appropriate if numerous family members present with similar corneal mosaic patterns.2
Currently, the significance of this finding remains unclear. Because it is an incidental and benign finding, it is likely underreported. Although it has been reported with other ocular disease entities in isolated cases, there is no clear association5-7. Future studies are needed to contribute to the understanding and significance of this disorder.
Faculty Approval by: Jeff Pettey, MD
References
- Vogt A. Lehrbuch Und Atlas Der Spaltlampenmikroskopie Des Lebenden Auges: Mit Anleitung Zur Technik Und Methodik Der Untersuchung. Technik Und Methodik. …. 1930.
- Belliveau MJ, Brownstein S, Agapitos P, Font RL. Ultrastructural Features of Posterior Crocodile Shagreen of the Cornea. Survey of Ophthalmology. 2009;54(5):569-575. doi:10.1016/j.survophthal.2009.02.022.
- Meyer JC, Quantock AJ, Kincaid MC, Thonar EJMA, Hageman GS, Assil KK. Characterization of a Central Corneal Cloudiness Sharing Features of Posterior Crocodile Shagreen and Central Cloudy Dystrophy of Francois. Cornea. 1996;15(4):347.
- Karp CL, Scott IU, Green WR, Chang TS. Central cloudy corneal dystrophy of François: a clinicopathologic study. Archives of …. 1997.
- Krachmer JH, Dubord PJ, Rodrigues MM, Mannis MJ. Corneal Posterior Crocodile Shagreen and Polymorphic Amyloid Degeneration: A Histopathologic Study. Arch Ophthalmol. 1983;101(1):54-59. doi:10.1001/archopht.1983.01040010056008.
- Bramsen T, Ehlers N, Baggesen LH. CENTRAL CLOUDY CORNEAL DYSTROPHY OF FRANÇOIS. Acta Ophthalmologica. 1976;54(2):221-226. doi:10.1111/j.1755-3768.1976.tb00435.x.
- Woodward M, Randleman JB, Larson PM. In Vivo Confocal Microscopy of Polymorphic Amyloid Degeneration and Posterior Crocodile Shagreen. Cornea. 2007;26(1):98-101. doi:10.1097/01.ico.0000240103.47508.c4.
Identifier: Moran_CORE_24263
Copyright statement: Copyright 2017. Please see terms of use page for more information.
Optic Nerve and Macular OCT in Hurler Syndrome (MPS I)
Home / Pediatric Ophthalmology and Strabismus / Ocular Manifestations of Systemic Disease
Title: Optic Nerve and Macular OCT in Hurler Syndrome (MPS I)
Author (s): Marshall J. Huang, BS
Photographer: Glen Jenkins
Date: 06/28/17
Images:
Keywords/Main Subjects: Hurler syndrome, Mucopolysaccharidosis, MPS, Optic disc edema
Diagnosis: Mucopolysaccharidosis Type I – Hurler Syndrome
Description of Image:
The images above include a photos of the optic nerve and SD-OCT of the macula in an 18-month male with a severe form of Mucopolysaccharidosis Type I (MPS I), also known as Hurler Syndrome. MPS I is an autosomal recessive, progressive, multisystem disorder caused by an absence or deficiency of the lysosomal enzyme α-L-iduronidase. This leads to a buildup of glycosaminoglycans within the lysosomes, resulting in a cascade of intracellular events that causes tissue damage and multi-organ dysfunction. This disease comprises of a spectrum of phenotypes, generally classified as Hurler (severe), Hurler-Scheie (intermediate), and Scheie (mild) syndromes.
Common systemic manifestations of Hurler syndrome include gargoyle facies, hepatospenomegaly, impaired cognitive development, dysostosis multiplex, and cardiorespiratory problems. Ocular manifestations include corneal opacification, pigmented retinopathy, central foveal ELM thickening, parafoveal IS/OS thinning, open angle glaucoma, and optic disc edema and atrophy. These symptoms can be delayed or even temporarily reversed using enzyme replacement therapy and hematopoietic stem cell transplant (HSCT).
This patient already received a HSCT but still had significant corneal clouding, as well as craniomegaly and hepatosplenomegaly. In order to evaluate the patient’s degree of retinal involvement, an exam under anesthesia was performed. Indirect ophthalmoscopy and photos of the optic nerve revealed significant disc edema in the left eye, a common finding in Hurler syndrome. In addition, SD-OCT of the macula showed early central foveal ELM thickening, greater in the left eye compared to the right. We also performed an electroretinogram (ERG) and visual evoked potentials (VEP). Those studies revealed significantly decreased flash ERG, 30Hz ERG, and flash VEP signals, with the left eye more attenuated than the right eye.
References:
- Parini R, Deodato F, Di Rocco M, et al. Open issues in Mucopolysaccharidosis type I-Hurler. June 2017:1-9. doi:10.1186/s13023-017-0662-9.
- Ana Maria Martins MD P, Ana Paula Dualibi MD P, Denise Norato MD P, et al. Guidelines for the Management of Mucopolysaccharidosis Type I. The Journal of Pediatrics. 2009;155(S):S32-S46. doi:10.1016/j.jpeds.2009.07.005.
Faculty Approval by: David C. Dries, MD; Griffin Jardine MD
Identifier: Moran_CORE_24253
Copyright statement: Copyright 2017. Please see terms of use page for more information.
Disclosure (Financial or other): None