Peripheral Leakage, Avascularity, and Non-perfusion –A Case of Familial Exudative Vitreoretinopathy
Home / Retina and Vitreous / Congenital and Developmental Abnormalities
Title: Peripheral Leakage, Avascularity, and Non-perfusion – A Case of Familial Exudative Vitreoretinopathy
Author (s): Blake H. Fortes, MSIV, Florida International University Herbert Wertheim College of Medicine
Photographer: Moran Eye Center
Date: 6/27/2018
Image or video:

Image 1: Montage color fundus photograph of the right eye demonstrating 1) a vitreous adhesion to the optic nerve with temporal macular traction, 2) vascular dragging and tortuosity, 3) far peripheral fibrotic changes overlying atrophic and pigmentary changes, and 4) exudates in the temporal periphery.
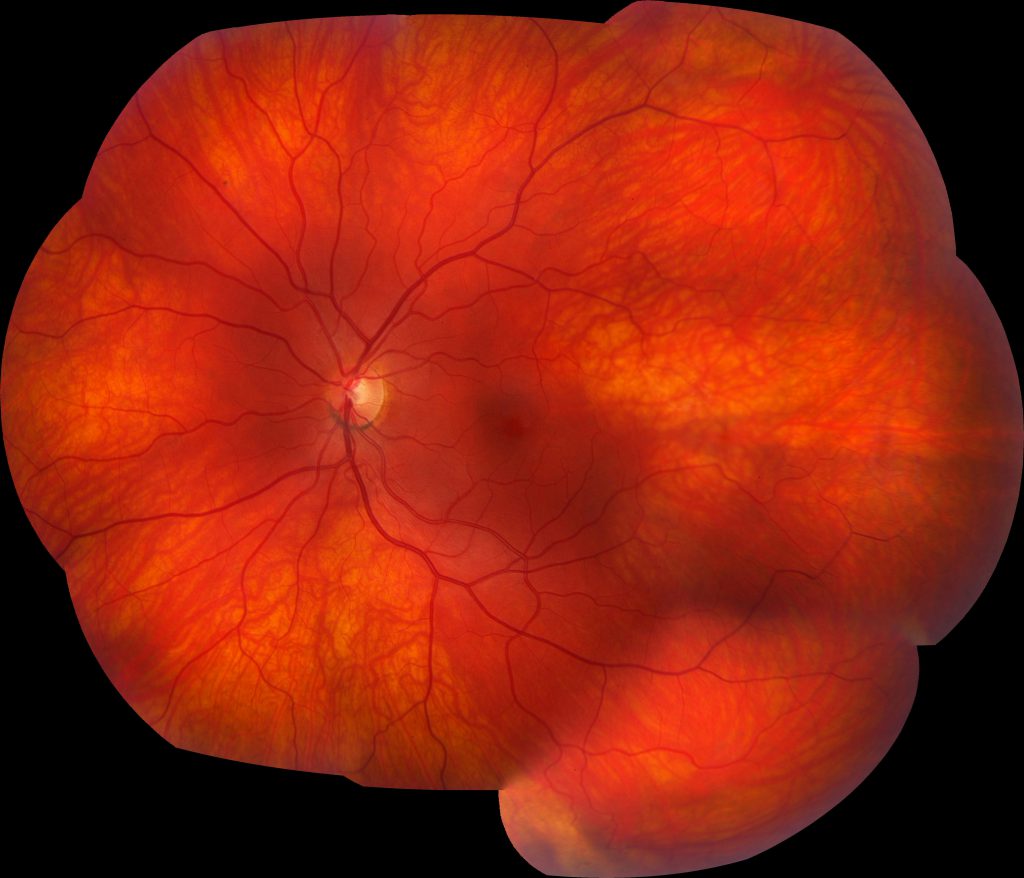
Image 2: Montage color fundus photograph of the left eye demonstrates a relatively normal fundus with some slight vascular tortuosity in the temporal periphery.
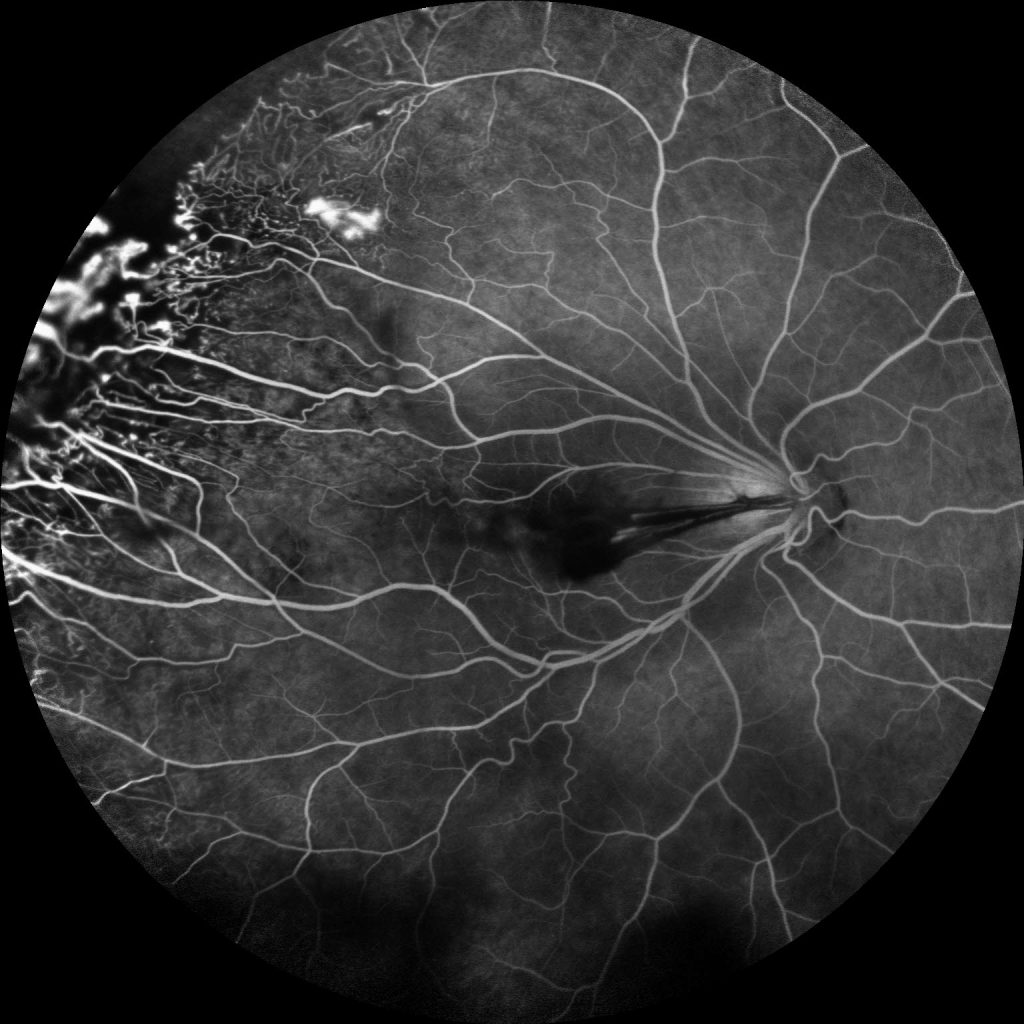
Image 3: Fluorescein angiogram of the right eye demonstrates multiple peripheral areas of focal hyperfluorescence that were shown to increase in intensity in the late phase along with diffuse leakage in the periphery and temporal peripheral non-perfusion.

Image 4: Fluorescein angiogram of the left eye revealing multiple areas of temporal vascular leakage with a broad temporal area of non-perfusion, which illustrates, not only, the importance of wide-field fluorescein angiography for diagnosing familial exudative vitreoretinopathy, but also the disease asymmetry that is characteristic of FEVR.
Keywords/Main Subjects: Familial exudative vitreoretinopathy, FEVR, peripheral avascularity, leakage, non-perfusion, neovascularization
Secondary CORE Category: Pediatric Ophthalmology and Strabismus / Disorders of the Retina and Vitreous
Diagnosis: Familial Exudative Vitreoretinopathy
Summary of Case: Patient is a 21 year old female with a diagnosis of a vasoproliferative tumor in the right eye who noted sudden onset of painless drastic decreased visual acuity in the right eye, which had drastically worsened over the last two months and was accompanied by floaters. She denied any photopsias. She has a history of myopia, and has always noticed decreased visual acuity in the right eye. She has no history of eye trauma, or surgery and was born at term, has a normal developmental history, and denied supplemental oxygen use at birth. Family ocular history was significant for a grandmother who had a retinal detachment requiring multiple surgeries. On exam, her visual acuity with correction in the right eye was 20/125 and in the left eye was 20/30 and was noted to have exotropia of the right eye. Her dilated fundus exam in the right eye revealed a tilted, small optic nerve with a vitreal adhesion from the disc to a temporal scar along with macular edema, temporal macular traction, epiretinal membrane, vascular dragging and tortuosity, as well as a fibrotic white lesion at 10 o’clock, surrounded by retinal pigment epithelial changes, and nearby exudates.
Familial Exudative Vitreoretinopathy:
FEVR is a disorder characterized by incomplete vascularization of the peripheral retina typically due to mutations in the Wnt signaling pathway, which is involved in organogenesis and angiogenesis of the eye. These gene mutations include NDP, FZD4, LRP5, and TSPAN12. Novel mutations in ZNF408 and KIF11 have recently been elucidated, but are not involved in the Wnt signaling pathway. The inheritance pattern varies depending on the mutation and may range from autosomal dominant (most commonly), to autosomal recessive, to X-linked recessive or even sporadic, as only 20-40% of patients with FEVR have a positive family history. Therefore, a negative family history does not exclude this diagnosis. This condition is characterized by variable expressivity and asymmetric disease.
The hallmark and most common finding of FEVR is avascularity in the temporal periphery of the retina with associated retinal neovascularization and fibrosis at the junction between the vascular and avascular retina. This fibrosis may result in traction of the macula and retinal vessels, resulting in macular dragging and radial retinal folds. Macular dragging may result in exotropia, as illustrated in this patient. Subretinal exudation, and any type of retinal detachment (rhegmatogenous, tractional, and exudative) may occur as well. Other less common findings associated with this disorder include secondary epiretinal membrane formation, vitreous hemorrhage, secondary glaucoma (neovascular or phacomorphic), retained hyaloid vascular remnants, and persistent fetal vasculature.
Differential diagnosis includes retinopathy of prematurity, Coats’ disease, Norrie’s disease, osteoporosis pseudoglioma syndrome, incontinentia pigmenti, persistent fetal vasculature, vasoproliferative tumor, and ocular toxocariasis.
The staging for FEVR includes:
- Stage 1: avascular periphery
- Stage 2: retinal neovascularization without exudate (A) or with exudate (B)
- Stage 3: extramacular retinal detachment without exudate (A) or with exudate (B)
- Stage 4: subtotal macula-involving retinal detachment without exudate (A) or with exudate (B)
- Stage 5: total retinal detachment
Only patients who have progressed significantly or are at high risk of progression should be treated. In stage 1-2A disease, the avascular retina should be treated with laser photocoagulation to decrease complications related to retinal neovascularization. Retinal detachment should be treated surgically via pars plana vitrectomy, scleral buckle, or a combination of these two approaches. Retinal exudation and neovascularization may also be managed adjunctively via intravitreal anti-VEGF injection prior to surgery. Due to the unpredictable course of FEVR, lifelong monitoring is indicated. Examination of family members is also warranted to reveal previously undiagnosed cases of FEVR.
Format: Case Presentation
References:
- Chen K, Wang N, Wu W. Familial Exudative Vitreoretinopathy. JAMA Ophthalmol. 2017;135(4):e165487. doi:10.1001/jamaophthalmol.2016.5487.
- Gilmour DF. Familial exudative vitreoretinopathy and related retinopathies. Eye. 2015;29(1):1-14. doi:10.1038/eye.2014.70.
- Natung T, Venkatesh P, Thangkhiew L, Syiem J. Asymmetric presentations of familial exudative vitreoretinopathy. Oman Journal of Ophthalmology. 2013;6(2):129-130. doi:10.4103/0974-620X.116661.
- Ranchod TM, Ho LY, Drenser KA, Capone A, and Trese MT. Clinical presentation of familial exudative vitreoretinopathy. Ophthalmology. 2011;118(10):2070-2075.
- Shastry, B. S. (2009), Persistent hyperplastic primary vitreous: congenital malformation of the eye. Clinical & Experimental Ophthalmology, 37: 884-890. doi:10.1111/j.1442-9071.2009.02150.x
- Shields CL, Kaliki S, Al-Dahmash S, et al. Retinal Vasoproliferative TumorsComparative Clinical Features of Primary vs Secondary Tumors in 334 Cases. JAMA Ophthalmol. 2013;131(3):328–334. doi:10.1001/2013.jamaophthalmol.524
- Sızmaz S, Yonekawa Y, T. Trese M. Familial Exudative Vitreoretinopathy. Turkish Journal of Ophthalmology. 2015;45(4):164-168. doi:10.4274/tjo.67699.
- Tauqeer Z, Yonekawa Y. Familial exudative vitreoretinopathy: Pathophysiology, diagnosis, and management. Asia Pac J Ophthalmol (Phila). 2018;7(3):176-182.
Faculty Approval by: Dr. Albert Vitale
Footer:
- Copyright statement: Copyright Author Name, ©2016. For further information regarding the rights to this collection, please visit: URL to copyright information page on Moran CORE
- Attribution/citation suggestions
Disclosure (Financial or other): None



