Fundus Photography, Fluorescein Angiography and Optical Coherence Tomography of Bilateral Exudative Detachments in a Pediatric Patient
Home / Pediatric Ophthalmology and Strabismus / Disorders of the Retina and Vitreous
Title: Fundus Photography, Fluorescein Angiography and Optical Coherence Tomography of Bilateral Exudative Detachments in a Pediatric Patient
Author: Olaoluwa Omotowa, MPH, Nnana Amakiri, MD, Marcus Altman, MD, Theresa Long, MD
Keywords/Main Subjects: Bilateral Exudative Retinal Detachments
Diagnosis: Bilateral Exudative Retinal Detachments
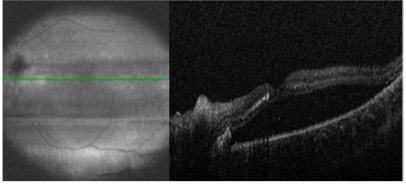
- Figure 1: Optical Coherence Tomography of Right Eye demonstrating inferior serous retinal detachment sparing the macula with optic disc edema.
- Figure 2: Optical Coherence Tomography of Left Eye demonstrating serous retinal detachment with macular involvement and optic disc edema.
- Figure 3: Color Fundus demonstrating Bilateral Serous Retinal Detachments with peripapillary cotton wool spots and full detachment of the macula OS. Elschnig spots in periphery OU.
- Figure 4: Fluorescein Angiography demonstrating patchy choroidal filling with scattered, nonspecific, hypofluorescent lesions with late hyperfluorescent lesions OU.
Description of Case:
A 4-year-old girl with a history of chronic hypertension, albinism, hypothyroidism, and complicated delivery requiring an extended NICU stay was referred to our facility with progressive ataxia, facial weakness, and loss of appetite. She was afebrile without new rashes or constitutional symptoms. The patient’s medical history included a seizure during NICU stay and a diagnosis of Bell’s Palsy at age 1. Additionally, she had a history of being diffusely edematous and hypertensive while in the NICU, which led to treatment with anti-hypertensive medications. At home her systolic blood pressures were reportedly in the 130-140s. Initial CT at an outside hospital revealed ventriculomegaly and brainstem glioma prompting urgent referral to our facility and neurosurgical consultation with administration of 4mg dexamethasone IV.
During her current presentation, she developed bilateral facial weakness, including ptosis related to Bell’s Palsy, along with her progressive ataxic gait, right ear pain, decreased appetite, and occasional emesis. On arrival, she had age-appropriate vital signs (94/58) and normal mental status.
Her neurological status deteriorated, necessitating an MRI scan. While lying flat in the MRI scanner, she became hypertensive with SBP in 180s. The scan revealed worsening ventriculomegaly, longitudinally extensive transverse myelitis, bilateral retinal hemorrhages, and nonenhancing T2/FLAIR signal in various brain regions. She received a total of 18 mg labetalol and ultimately required nicardipine drip 1.5 mcg/kg/hr normalizing her blood pressure to 138/100. She was intubated in MRI and taken for emergent EVD placement with neurosurgery. She tolerated the procedure well without complications and was subsequently weaned off her nicardipine drip. Given the ocular findings on imaging, ophthalmology was promptly consulted.
Ophthalmic examination revealed no light perception in both eyes both of which were soft to palpation. She had mild esophoria and no afferent pupillary defect though was on miotics. Her fundus examination revealed bilateral exudative retinal detachments, tortuous vessels, and diffuse serous detachments with a tigroid appearance and diffuse creamy infiltrates. Further evaluation, including ocular ultrasonography and fluorescein angiography, was performed to ascertain the underlying cause.
A comprehensive workup, including laboratory investigations, lumbar puncture, whole-genome sequencing, and whole body imaging was initiated to identify the etiology of the bilateral exudative retinal detachments. Laboratory results indicated AQP4-IgG, Adams13, MOG Ab IgG, D-dimer, Haptoglobin, RPR, TSH, C3, C4 CRP, and ESR were within normal limits. RCIGM revealed no genomic variants. Anti-CFH Autoantibody, HSV IgG/IgM, B Burgdorferi IgM & IgG, Quant Gold, Cat Scratch IgG & IgM, ANCA, HIV, Treponema, meningitis/encephalitis panel, oligoclonal bands, CSF flow and cytology were negative. LDH (740), platelets (316), IgG (333), IgG synthesis (14.5), and Von Willebrand Ag (150%) were all elevated. The patient’s clinical and diagnostic findings led to a diagnosis of hypertensive chorioretinopathy as the most likely cause.
Patient was scheduled for close follow up 2 weeks after her initial diagnosis. After not making it to this appointment she was rescheduled with her hometown ophthalmologist. These visits demonstrated gradual resolution of subretinal fluid and exudates. Serial optical coherence tomography scans and dilated examinations demonstrated reattachment of the retina in both eyes, with the patient’s visual acuity improving, although some residual impairment remained due to macular involvement. She was 20/300 in her right eye and 20/200 in her left.
Summary of the Case:
- Bilateral exudative retinal detachments in pediatric patients present diagnostic challenges due to their rarity and various potential etiologies.
- The causes can be classified as inflammatory, infectious, or neoplastic, including conditions like familial exudative vitreoretinopathy, hemolytic uremic syndrome, choroidal lymphoma, hemangioma, and metastases.
- The presented case highlights the importance of considering rare causes, such as malignant hypertension, in patients with bilateral exudative retinal detachments. Prompt control of blood pressure played a crucial role in the resolution of fundus findings.
- This case emphasizes the significance of thorough evaluation and heightened awareness among eyecare providers when encountering pediatric patients with bilateral exudative retinal detachments. Timely diagnosis and management are crucial to prevent irreversible vision loss.
- Hypertensive chorioretinopathy should be considered as a possible etiology in cases of acute on chronic hypertension presenting with retinal detachments.
References:
- Yoshida, K., Hasegawa, D., Takusagawa, A., Kato, I., Ogawa, C., Echizen, N., … & Manabe, A. (2010). Bullous exudative retinal detachment due to infiltration of leukemic cells in a child with acute lymphoblastic leukemia. International journal of hematology, 92, 535-537.
- Rosecan, L. R., Laskin, O. L., Kalman, C. M., Haik, B. G., & Ellsworth, R. M. (1986). Antiviral therapy with ganciclovir for cytomegalovirus retinitis and bilateral exudative retinal detachments in an immunocompromised child. Ophthalmology, 93(11), 1401-1407.
- Navarrete, A., Jaouni, T., & Amer, R. (2023). Total exudative retinal detachment in a child with pars planitis-a challenging case with optimistic results. Journal of Ophthalmic Inflammation and Infection, 13(1), 1-4.
- Otuka, O. A. I., Eweputanna, L. I., Okoronkwo, N. C., & Kalu, A. (2021). Bilateral Exudative Retinal Detachment in a Young Patient with Chronic Renal Failure. International Medical Case Reports Journal, 139-144.
- Khaja, W. A., Pogrebniak, A. E., & Bolling, J. P. (2015). Combined orbital proptosis and exudative retinal detachment as initial manifestations of acute myeloid leukemia. Journal of American Association for Pediatric Ophthalmology and Strabismus, 19(5), 479-
- Shukla UV, Gupta A, Tripathy K. Exudative Retinal Detachment. 2023 Feb 22. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 36944005.
Faculty Approval by: Theresa Long, MD
Copyright statement: Olaoluwa Omotowa, ©2023. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/