Optic Disc Pit: Pathogenesis, Presentation, Imaging, and Management Overview
Title: Optic Disc Pit: Pathogenesis, Presentation, Imaging, and Management Overview
Author: Leo Meller, BS
Date: 09/12/2025
Images:
Keywords/Main Subjects: Optic Disc Pit, Optic Disc Pit Maculopathy
Diagnosis: Optic Disc Pit
Description of Image:
Optic disc pit is a rare congenital optic disc anomaly with an estimated prevalence of 1 in 11,000.1 While its embryological process remains the topic of investigation, it is most commonly believed to arise secondary to abnormal primordial optic nerve papilla development and remnant of peripapillary neuroectodermal folds.2 The majority of cases are unilateral (85%), sporadic, have no gender predisposition, and stand alone or in association with optic disc colobomas.1 On fundus exam, they are most often described as an oval-shaped, grey-white depression in the inferotemporal disc with sizes ranging from 1/10 to 7/10 of the disc.1
While most patients are asymptomatic with the anomaly detected incidentally on fundus exam, a subset of patients may develop optic disc pit maculopathy due to intra- and subretinal fluid accumulation3 that most often onsets between the age of 30-40.4 Multiple competing theories exist regarding the fluid origin, whether it is from the vitreous, leakage from surrounding blood vessels at the pit, cerebrospinal fluid, or dura,5 and fluid leakage has been mainly attributed to vitreous traction given the strong co-occurrence of optic disc pit maculopathy and posterior vitreous detachment.6 Clinically, these patients often present with worsening visual acuity beyond 20/70 along with declining visual field and color vision,3 and diagnosis is established based on fundus and macular OCT imaging.5 While there is a lack of consensus on best treatment for optic disc pit maculopathy given the disease rarity, pars plana vitrectomy (23-gauge) is a commonly accepted treatment modality with studies demonstrating visual acuity improvement in over half of the cases and success rate between 50-95%.7 The vitrectomy is followed by a surgically induced posterior vitreous detachment for traction release and macular reattachment.3 Other proposed treatment options include pneumatic tamponade, macular buckling, and modalities to patch the pit with materials such as fibrin glue, internal limiting membrane flaps, human amniotic membrane patches or autologous scleral flaps.8 Factors associated with worse prognosis include metamorphopsia, delayed vitrectomy, and worse visual acuity at presentation.9 Interestingly, pit location and size were not associated with prognosis.9
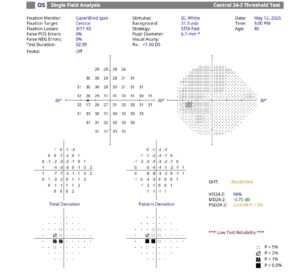
Herein, we present a 41 y/o male with a history of LASIK who was referred to glaucoma from optometry for an anomalous optic nerve without vision complaints. His visual acuity was 20/25 OD, 20/20 OS, with IOP <15 OU. Fundus exam of the right eye was normal, whereas the left eye showed an optic disc pit inferior temporally with oval hypopigmentation. 24-2 of the left eye showed central visual field loss, with RNFL demonstrating corresponding temporal thinning. OCT macula of the left eye demonstrated trace intraretinal fluid with IS/OS junction loss. His visual field, RNFL and macular OCT of the right eye was normal. Given his un-changed VA at the 9 month follow up, no vision concerns and no significant maculopathy, he is recommended to return for follow up in 8 months with repeat fundus exam, visual field, and RNFL and macular OCT.
References:
- Uzel MM, Karacorlu M. Optic disk pits and optic disk pit maculopathy: A review. Survey of Ophthalmology. 2019;64(5):595-607. doi:10.1016/j.survophthal.2019.02.006
- Gass JD. Serous detachment of the macula. Secondary to congenital pit of the optic nervehead. Am J Ophthalmol. 1969;67(6):821-841. doi:10.1016/0002-9394(69)90075-0
- Kalogeropoulos D, Ch’ng SW, Lee R, et al. Optic Disc Pit Maculopathy: A Review. The Asia-Pacific Journal of Ophthalmology. 2019;8(3):247. doi:10.22608/APO.2018473
- Brodsky MC. Congenital optic disk anomalies. Surv Ophthalmol. 1994;39(2):89-112. doi:10.1016/0039-6257(94)90155-4
- Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: a review. Graefes Arch Clin Exp Ophthalmol. 2011;249(8):1113-1122. doi:10.1007/s00417-011-1698-5
- Shah SD, Yee KK, Fortun JA, Albini T. Optic Disc Pit Maculopathy: A Review and Update on Imaging and Treatment. International Ophthalmology Clinics. 2014;54(2):61. doi:10.1097/IIO.0000000000000025
- Chatziralli I, Theodossiadis P, Theodossiadis GP. Optic disk pit maculopathy: current management strategies. Clin Ophthalmol. 2018;12:1417-1422. doi:10.2147/OPTH.S153711
- Caporossi T, D’Amico G, Tartaro R, et al. Optic Disk Pit Maculopathy Treatment Using a Human Amniotic Membrane Patch: One-Year Results. American Journal of Ophthalmology. 2022;240:30-36. doi:10.1016/j.ajo.2022.02.014
- Kang HG, Kim JD, Lee J, Byeon SH, Kim SS, Kim M. Clinical features, treatment factors, and long-term outcomes of optic disc pit maculopathy. Graefes Arch Clin Exp Ophthalmol. 2022;260(9):2867-2875. doi:10.1007/s00417-022-05661-2
Faculty Approval by: Brian Stagg, MD
Copyright statement: Copyright Leo Meller, ©2025. For further information regarding the rights to this collection, please visit: URL to copyright information page on Moran CORE