Lens-Induced Glaucoma: Overview and Case Report
Title: Lens-Induced Glaucoma: Overview and Case Report
Authors: Bryce Baugh, MSIV, University of Utah Spencer Fox Eccles School of Medicine, Austin Nakatsuka, MD
Date: 08/27/2024
Keywords/Main Subjects: lens-induced glaucoma, phacomorphic glaucoma, phacolytic glaucoma, phacoantigenic glaucoma, lens-particle glaucoma
Diagnosis: Phacomorphic Glaucoma
Description of Case:
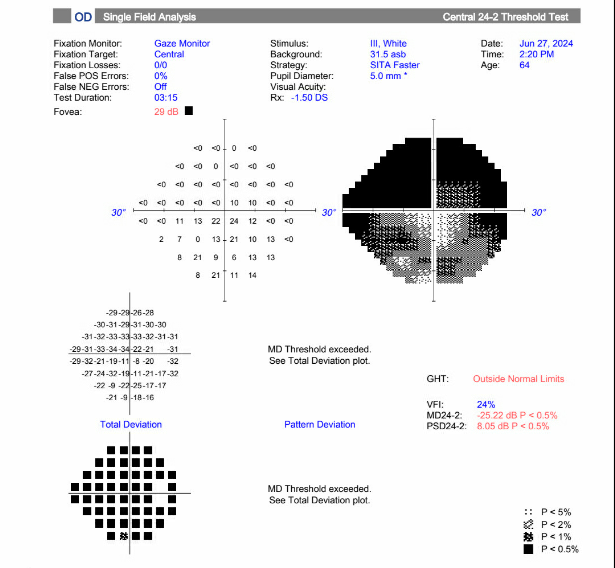
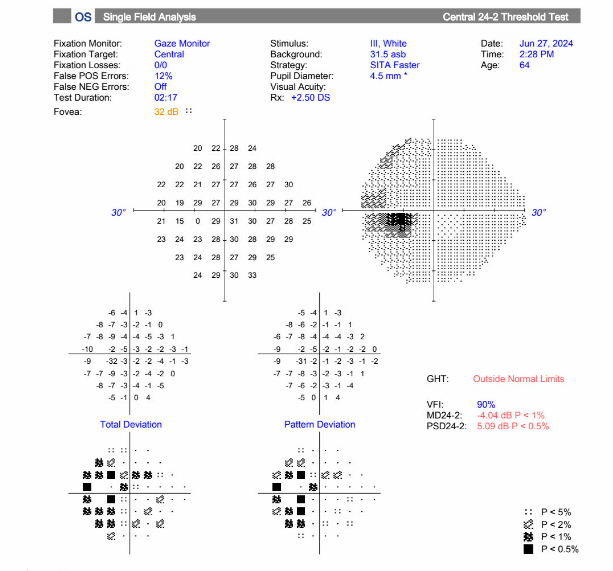
A 64-year-old male presented with five days of acute vision loss and light sensitivity in the right eye. The patient reported that when he awoke in the morning five days prior, he was unable to see out of his right eye. The patient denied any pain or irritation but noted an increased pressure sensation in his right eye. He denied any redness or discharge. Since initial onset, his vision had slightly improved. His ocular history was notable for retinal detachment 20 years prior with cryotherapy. Ocular history was also notable for LASIK more than 20 years prior complicated by increased IOP due to a steroid response following surgery. Other past medical history was non-contributory. The patient’s visual acuity at initial presentation was 20/80 in the right eye, 20/30 in the left eye. Applanation revealed a pressure of 40 in the right eye, 10 in the left eye. Gonioscopy showed A20b in the right eye and C35f 2+ptm in the left eye circumferentially. Visual field defects in right superonasal and superotemporal fields were noted. Slit lamp exam of the right eye showed trace conjunctival injection, hazy cornea, very narrow anterior chamber, and 2+ nuclear sclerosis and 2+ cortical cataract. The fundus exam showed tilted disc, with tilted cup and small optic nerve, and significant nasal peripapillary atrophy. The left eye showed 1+ nuclear sclerosis and was otherwise normal.
The decision was made to proceed with laser peripheral iridotomy of the right eye for treatment of acute angle closure glaucoma, likely phacomorphic in nature. Following iridotomy, the patient was instructed to continue Cosopt and Brimonidine twice daily in the right eye, as well as acetazolamide 500mg twice daily. The following day, the pressure in the right eye was 7 and visual acuity was 20/70. The anterior chamber still appeared narrow, but now appeared more even centrally and peripherally. The patient was instructed to continue all medications. At follow up the following week, the patient’s vision had improved to 20/30 and pressure in the right eye was 11. With pressures now under control but persistently shallow-appearing anterior chamber and mature cataract, the patient was scheduled for phacoemulsification and IOL placement with goniotomy and anterior vitrectomy of the right eye. This took place approximately 1 month after the patient’s initial presentation.
Intraoperatively, it was noted that the patient had a very shallow anterior chamber, with little space to even make corneal incisions. During phacoemulsification, it was noted that the lens capsule had significant global zonular laxity necessitating the placement of a capsular tension ring before lens placement. A nasal 3-4 clock hour goniotomy with the Kahook Dual Blade was done after the phacoemulsification and lens placement were completed. Please see attached surgical video with narration for more details.
At the patients first postoperative visit 1 week following surgery, pinhole visual acuity was 20/60 in the right eye, and pressure was 15. The anterior chamber appeared deep, with 1+ cell. The patient was continued on brimonidine BID OD, and prednisolone BID OD for 2 weeks. The patient appears clinically improved and will continue to be monitored at subsequent follow up appointments.
Overview:
Lens-induced glaucoma is form of secondary glaucoma where the ocular lens is directly involved in the mechanism contributing to increased intra-ocular pressure (IOP). It is one of the most common types of secondary glaucoma presenting with a senile cataract. There are thought to be four primary processes through which this can occur–one involving aqueous obstruction, and the others being lens-protein associated. The different etiologies include phacomorphic, phacolytic, lens-particle associated, and phacoantigenic. The pathogenesis, clinical features, and management are outlined below.
Pathogenesis:
Phacomorphic glaucoma is the most common type of lens-induced glaucoma and involves a sudden increase in the volume of the cataract lens. The intumescent lens can lead to pupillary block and disruption of aqueous humor flow from the posterior to anterior chamber. As pressure builds in the posterior chamber, the iris is pushed forward, obstructing outflow through the trabecular meshwork and causing acute angle closure.1
Phacolytic glaucoma is thought to involve obstruction of the trabecular meshwork by macrophages and typically occurs in the setting of a mature senile cataract. High molecular weight proteins leak into the anterior chamber from microdefects in the lens capsule. The macrophages attempting to phagocytose these proteins block the trabecular meshwork, resulting in an open-angle glaucoma.2
Lens-particle glaucoma typically presents following trauma, cataract surgery, or YAG capsulotomy. As lens fragments are left behind, they migrate and deposit in the trabecular meshwork, resulting in obstruction of outflow and an open-angle glaucoma.
Phacoantigenic glaucoma is a type III hypersensitivity reaction and typically presents 1-14 days following cataract surgery.3 It is normally associated with a complicated cataract surgery involving the mixture of lens and vitreous.4 As lens particles are released, there is a sensitization period where immune complexes are formed. The reaction promotes inflammatory cells which subsequently block the trabecular meshwork causing open-angle glaucoma.
Clinical Features:
| Symptoms | Signs | |
| Phacomorphic Glaucoma |
· Severe eye pain
· Blurry vision · Eye redness · Headache · Nausea/vomiting
|
· Conjunctival injection
· Corneal edema · Mid-dilated pupil · Intumescent lens pushing iris forward · Decreased AC depth
|
| Phacolytic Glaucoma |
· Severe eye pain
· Blurry vision · Eye redness
|
· Corneal edema
· Fresh karatitic precipitates on posterior surface of cornea · AC cell and flare · Hyper-refringent particles composed of calcium oxalate or cholesterol crystals5 · Anterior peripheral/posterior synechiae · Hypermature cataract
|
| Lens-Particle Glaucoma |
· Severe eye pain following trauma or surgery
· Blurry vision · Eye redness |
· Conjunctival injection
· Corneal edema · Anterior peripheral/posterior synechiae · Lens proteins deposited on posterior surface of cornea · Lens particles in AC · Rupture of the lens capsule with a cataractous lens may be present
|
| Phacoantigenic Glaucoma |
· Severe eye pain
· Blurry vision · Eye redness
|
· Eyelid edema
· Conjunctival injection · Corneal edema · Fresh karatitic precipitates on posterior surface of cornea · AC cell and flare · Anterior peripheral/posterior synechiae · Ruptured lens capsule vs. anterior capsulorrhexis with residual lens matter
|
Diagnostic tools:
- Applanation tonometry
- Gonioscopy
- B-scan if view of posterior segment limited
Treatment:
Phacomorphic Glaucoma:
- Lower IOP with aqueous suppressants or hyperosmotic agents
- Consider laser iridotomy
- Cataract surgery once IOP lowers and inflammation resides
Phacolytic Glaucoma:
- Topical steroids
- Topical aqueous suppressants to lower IOP
- Cataract surgery is definitive treatment
Lens-particle Glaucoma:
- If there is minimal cortical material: topical steroids, cycloplegics, topical aqueous suppressants
- If significant inflammation and IOP can’t be lowered quickly: early removal of residual lens cortex via irrigation or vitrectomy
Phacoantigenic Glaucoma:
- Topical steroids
- Topical aqueous suppressants to lower IOP
- Possible surgery to remove remanent lens material
Images or video:
- Images: Visual field of the right eye showing significant defect, most severe in the superonasal and superotemporal fields.
- Video: https://www.youtube.com/watch?app=desktop&v=j-NwR04ZJUI
- Narrated surgical video of cataract extraction and goniotomy in a patient with phacomorphic glaucoma.
Summary of the Case: Lens-induced glaucoma is form of secondary glaucoma where the ocular lens is directly involved in the mechanism contributing to increased intra-ocular pressure (IOP). The most common etiology is phacomorphic and other etiologies include phacolytic, lens-particle associated, and phacoantigenic. The presentation varies between etiologies, but largely presents with eye pain, blurry vision, eye inflammation, increased IOP, mature cataract, or following cataract surgery. Treatment focuses on timely reduction of IOP, minimizing inflammation, and eventual cataract surgery.
References:
- Ellant JP, Obstbaum SA. Lens-induced glaucoma. Doc Ophthalmol. 1992;81(3):317-338. doi:10.1007/BF00161770
- Epstein DL, Jedziniak JA, Grant WM. Obstruction of aqueous outflow by lens particles and by heavy-molecular-weight soluble lens proteins. Invest Ophthalmol Vis Sci. 1978;17(3):272-277.
- Perlman EM, Albert DM. Clinically unsuspected phacoanaphylaxis after ocular trauma. Arch Ophthalmol. 1977;95(2):244-246. doi:10.1001/archopht.1977.04450020045008
- Conner IP et al. Lens-induced glaucoma. In: Kahook M et al, eds. Chandler and Grant’s Glaucoma, 5th ed. Thorofare, N.J.; Slack; 2013:441-447
- Peracha-Riyaz MH, Peracha ZH, Spaulding J, et al. First Described Case of Anterior and Posterior Segment Crystals in Phacolytic Glaucoma. J Glaucoma. 2017;26(5):e171-e173. doi:10.1097/IJG.0000000000000642
Faculty Approval by: Austin Nakatsuka
Copyright statement: Bryce Baugh, ©2024. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/