Intraocular Pressure Fluctuation in a Patient with Pseudoexfoliation Glaucoma
Title: Intraocular Pressure Fluctuation in a Patient with Pseudoexfoliation Glaucoma
Authors: Tara Gallant, California Northstate University College of Medicine, MD Class of 2024; Barbara Wirostko, MD
Date: September 2023
Keywords/Main Subjects: Pseudoexfoliation Syndrome, Pseudoexfoliation Glaucoma, Intraocular Pressure Fluctuations, Home iCare
Introduction:
Pseudoexfoliation syndrome (XFS) results from abnormal fibrillar extracellular material accumulation in ocular tissues, including all structures of the anterior segment, the conjunctiva, and orbital structures.1 XFS is one of the most common causes of open-angle glaucoma. Pseudoexfoliation glaucoma (XFG) typically presents with a higher maximum and mean IOP at the time of diagnosis, as well as a wider range of IOP fluctuation, compared with primary open angle glaucoma (POAG). It is associated with a higher risk of progressive vision loss than POAG, more rapidly developing cataracts, phacodenesis, lens subluxation, and retinal vascular events.1,2 XFS manifestations are age-related and estimated to be present in 10-20% of the general population above the age of 60 depending upon the geographic location.2 Patients with XFS are thought to have a ten-fold higher risk of developing glaucoma than the general population.2 On dilated clinical exam, XFS can be identified by the presence of white deposits on the anterior lens surface and pupillary margins. Ultrasound biomicroscopy often reveals zonular weakness, a thickened lens, a narrow anterior chamber, and occludable angles.2 Systemic diseases with an increased incidence in patients with XFS include chronic obstructive pulmonary disease, inguinal hernias, pelvic organ prolapse, obstructive sleep apnea, and atrial fibrillation.3
Case Presentation:
Our patient is an 81-year-old female with severe stage capsular pseudoexfoliation glaucoma in both eyes. Five years ago, she underwent Phaco CyPASS surgeries in both eyes. Approximately two years ago, the patient had a XEN gel stent with mitomycin C/Ologen placed in the right eye. Her current ocular medications include Cosopt BID OU and Vyzulta QHS OU. Other ocular conditions include dry eye syndrome and meibomitis. She has a history of pelvic organ prolapse, and her mother was also diagnosed with glaucoma and pelvic organ prolapse.
At her most recent visit, visual acuity was 20/30 OD and 20/25 OS, with applanation tonometry readings of 8 OD and 12 OS. Slit lamp exam was notable for pseudoexfoliation material on the anterior aspect of the lens capsule with no transillumination defects bilaterally. She was also noted to have phacodenesis OD. Her right optic nerve had temporal pallor and a cup/disc ratio of 0.95, and her left optic nerve had an infratemporal notch with a cup/disc ratio of 0.6. Other exam findings included trace meibomian gland dysfunction OU, trace hordeolum OU, and well-centered posterior chamber intraocular lenses bilaterally. Optic nerve OCT scans demonstrated diffuse temporal thinning OD and infratemporal thinning OS, with no progression of glaucomatous damage over the past year and a half in either eye when compared to prior scans.
Two and a half years ago, the patient was assigned an iCare HOME to determine if she was experiencing intraocular pressure (IOP) fluctuations that could help explain the severe and progressive glaucomatous damage to her optic nerves, particularly in her right eye. A summary of the results is shown in Figure 1 below. The measurements taken revealed higher overall IOP in the right eye outside of normal clinic hours, as well as increased fluctuation in pressures when compared to the left eye. The highest and lowest measurements taken are shown in Table 1 below.
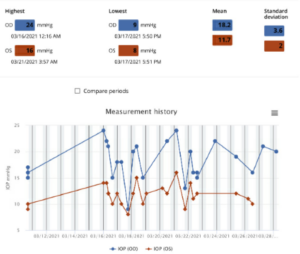
Figure 1: Summary of the results of iCare Home measurements taken three months prior to the glaucoma stent procedure OD. All the measurements were “excellent” in quality. Average IOP and variability of IOP was higher in the right eye, which had more glaucomatous damage compared to the left eye. Both average IOP and variability of IOP in OD were higher on these iCare measurements than on clinical measurements around the same time.
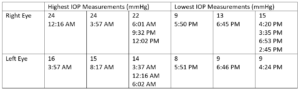
Table 1: Highest and lowest IOP measurements taken in each eye while the patient had the iCare HOME and the corresponding times at which the measurements were taken three months prior to the glaucoma stent procedure OD. Notably, the highest IOP measurements were recorded overnight and in the morning, whereas the lowest IOP measurements were recorded in the afternoon and early evening.
The decision was made to perform additional surgery in the right eye three months after those initial iCare measurements were taken to better control IOP fluctuations, as the patient had pericentral visual field loss OD (Figure 2) and diffuse optic nerve thinning temporally OD (Figure 3).
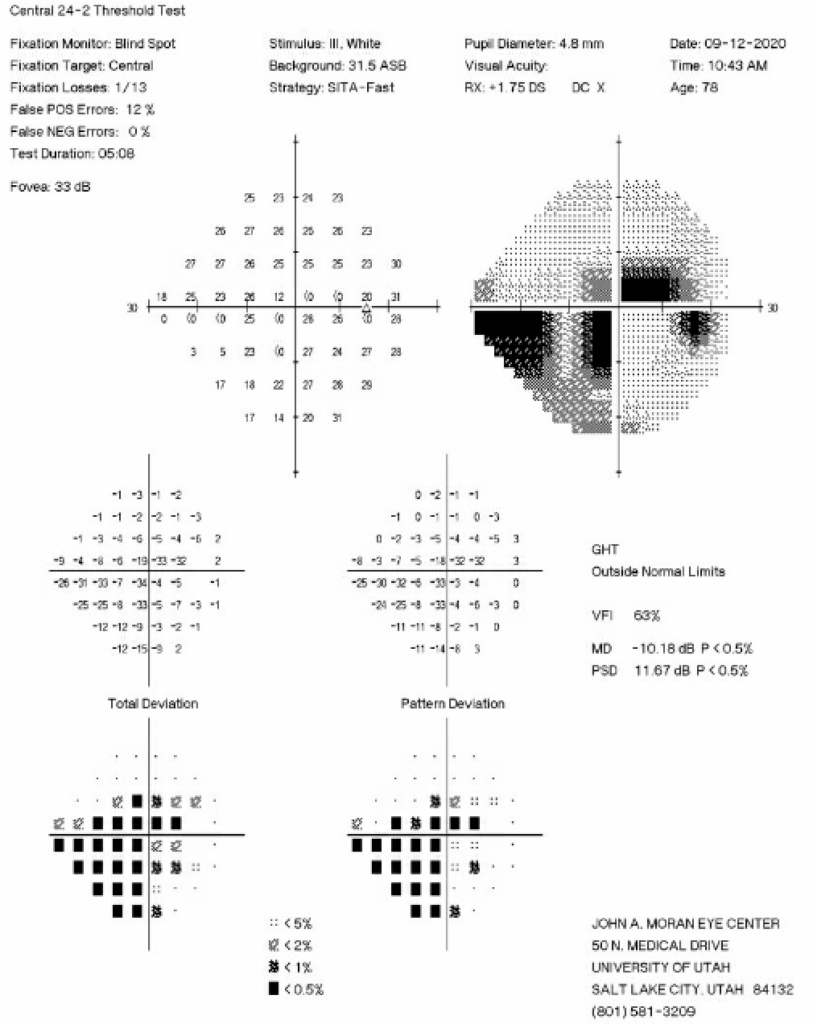
Figure 2: 24-2 Humphrey Visual Field test from six months prior to the initial iCare HOME measurements showing an inferior nasal step and pericentral visual field loss in the right eye.
Nine months after the XEN gel stent with mitomycin C/Ologen was placed in the right eye, the patient was asked to repeat the iCare measurements. A summary of the results is shown in Figure 4 below.

Figure 4: Summary of the results of iCare HOME measurements taken nine months after the glaucoma stent procedure OD. All the measurements were “excellent” in quality. Average IOP and variability of IOP in the right eye were now both lower compared to the iCare HOME measurements from one year prior.
Discussion:
IOP varies both daily and hourly, and clinicians are not able to fully understand patients’ IOP when only capturing measurements at office visits. In a study conducted at the Wilmer Eye Institute, it was found that mean IOP was slightly lower by home tonometry readings than by clinic readings alone, while IOP fluctuation and IOP spikes were significantly higher than those measured in clinic.4 Additionally, those researchers found that mean daily measurements exceeded the recent clinic maximum IOP in 44% of patients, and that mean daily measurements by home iCare were greater than any historic IOP measured in clinic in 13% of patients.4 Furthermore, the peak home IOP occurred outside of the typical 8:00 am – 5:00 pm office hours on half of the days.4 Diurnal IOP fluctuations have been documented dating back several decades. In one study analyzing 2272 diurnal curves of IOP measurements, 41% of the peaks were found at the early morning IOP measurement, while 24% of peaks were found at the second, mid-morning measurement.5 Another study showed this pattern of nocturnal IOP elevation occurs independently of central corneal thickness, corneal hysteresis, and corneal resistance factor.6
Mean IOP and diurnal fluctuation in IOP are typically higher in XFG than in POAG, and reduction of these measures has been documented to be more effective in XFG than in POAG in preventing visual field damage.7 In our patient, implanting a XEN gel stent with mitomycin C/Ologen in the eye with significant glaucoma damage lowered her average home iCare reading in that eye from 18.2 to 9.5, and the standard deviation of IOP measures decreased from 3.6 to 1.0. With these significantly improved eye pressures, RNFL thickness and visual fields have remained relatively stable for the past two years since her surgery. This case demonstrates the importance of understanding how IOP varies throughout the day, and the efficacy of surgical intervention on minimizing both fluctuations in these measurements and glaucomatous changes in the eye.
References:
-
- Ritch R, Schlötzer-Schrehardt U. Exfoliation syndrome. Surv Ophthalmol. 2001;45(4):265-315. doi:10.1016/s0039-6257(00)00196-x
- Yüksel N, Yılmaz Tuğan B. Pseudoexfoliation Glaucoma: Clinical Presentation and Therapeutic Options. Turk J Ophthalmol. 2023;53(4):247-256. doi:10.4274/tjo.galenos.2023.76300
- Pompoco CJ, Curtin K, Taylor S, et al. Summary of Utah Project on Exfoliation Syndrome (UPEXS): using a large database to identify systemic comorbidities. BMJ Open Ophthalmol. 2021;6(1):e000803. doi:10.1136/bmjophth-2021-000803
- McGlumphy EJ, Mihailovic A, Ramulu PY, Johnson TV. Home Self-tonometry Trials Compared with Clinic Tonometry in Patients with Glaucoma. Ophthalmol Glaucoma. 2021;4(6):569-580. doi:10.1016/j.ogla.2021.03.017
- David R, Zangwill L, Briscoe D, Dagan M, Yagev R, Yassur Y. Diurnal intraocular pressure variations: an analysis of 690 diurnal curves. Br J Ophthalmol. 1992;76(5):280-283.
- Bagga H, Liu JHK, Weinreb RN. Intraocular pressure measurements throughout the 24 h. Curr Opin Ophthalmol. 2009;20(2):79-83. doi:10.1097/ICU.0b013e32831eef4f
- Vahedian Z, Salmanroghani R, Fakhraie G, et al. Pseudoexfoliation syndrome: Effect of phacoemulsification on intraocular pressure and its diurnal variation. J Curr Ophthalmol. 2015;27(1-2):12-15. doi:10.1016/j.joco.2015.09.006
Identifier: Moran_CORE_127006
Copyright: Tara Gallant and Barbara Wirostko ©2023. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/



