Uveitic Cataract in Biopsy-proven Sarcoid-associated Uveitis
Home / Intraocular Inflammation and Uveitis / Complications of Uveitis
Title: Uveitic Cataract in Biopsy-proven Sarcoid-associated Uveitis
Authors: Amanda Wade, BA; Marissa Larochelle, MD
Date: 07/18/2024
Keywords/Main Subjects: uveitis, cataracts, uveitic cataract, uveitis complications, ocular sarcoidosis
Diagnosis: Cataract secondary to uveitis
Description of Case: A 46-year-old woman with biopsy-proven sarcoid-associated uveitis complicated by bilateral peripapillary and macular CNVM (choroidal neovascular membrane) with submacular fibrosis presented with gradually decreasing vision over the previous year in the left eye.
Initial ocular presentation occurred approximately 20 years prior with bilateral eye pain and redness (anterior sarcoid uveitis). She was followed for “macular degeneration” at the time due to posterior involvement appreciated on exam and received laser (PDT) over the course of multiple visits. She then transitioned care to another physician who proceeded with Avastin injections for about 1 year. She eventually began methotrexate for systemic control of her sarcoidosis.
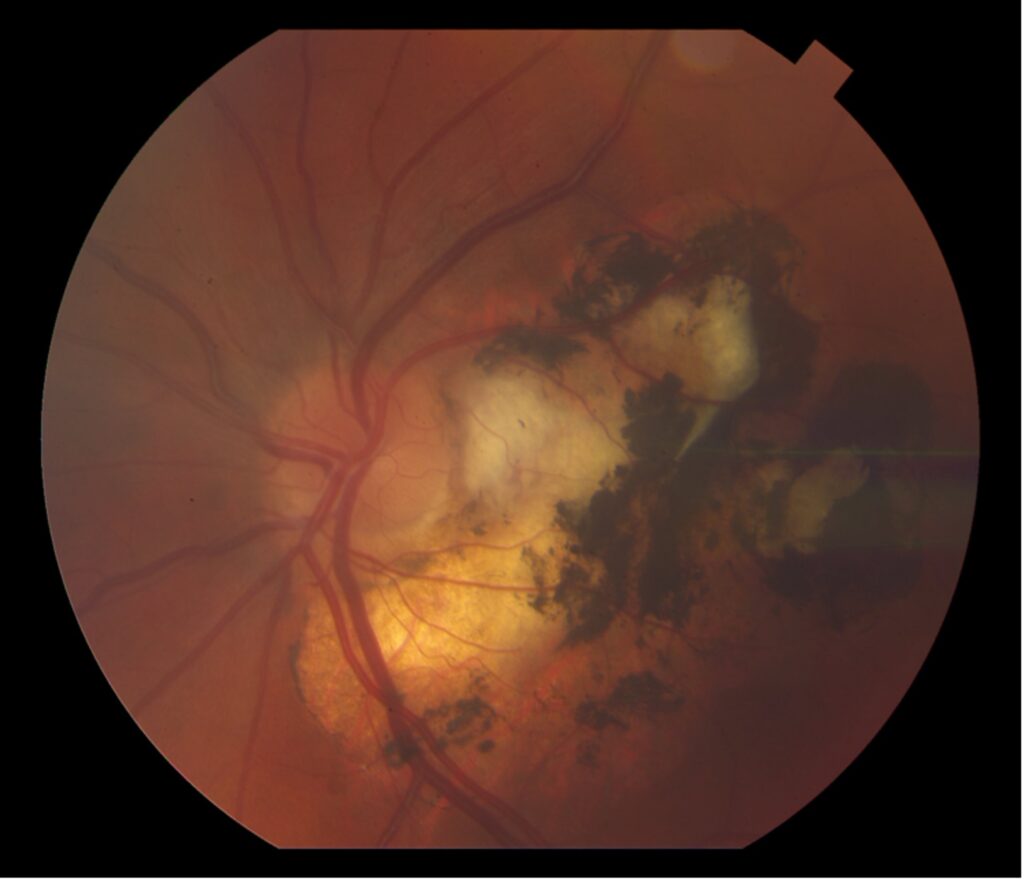
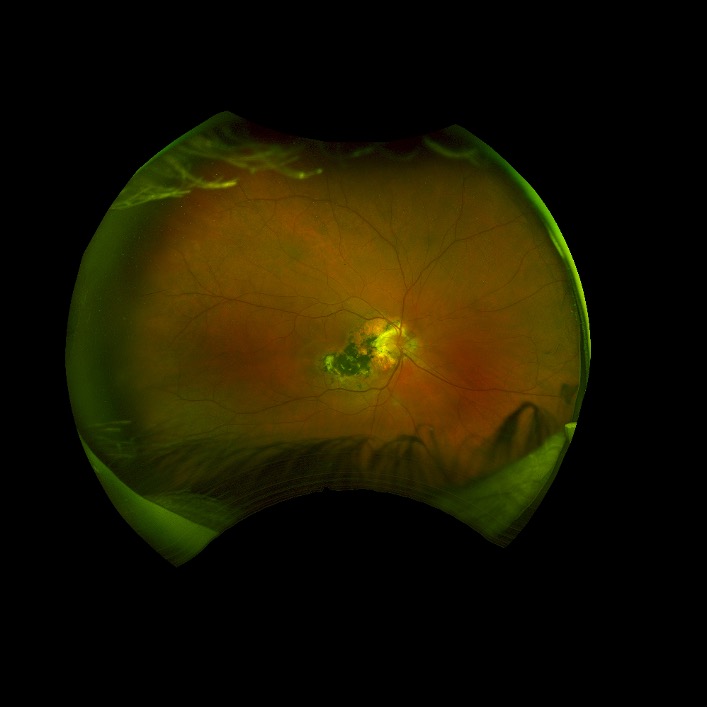
Figure 1. Fundus photos:
Peripapillary and macular CNVM pictured in both right and left eyes; notably clear view of the fundus bilaterally.
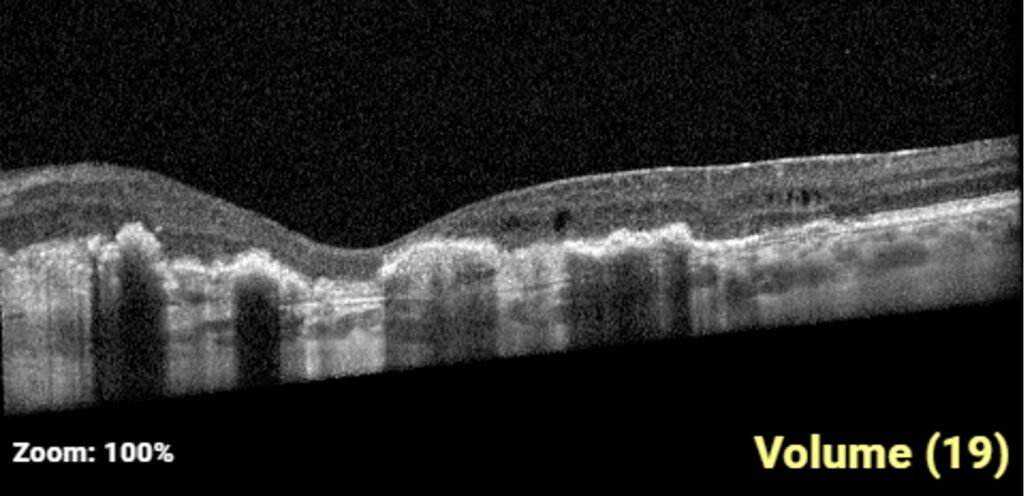
Figure 2. Macula OCT – left eye:
Sub retinal hyperreflectivity, intraretinal hyperreflectivity, multiple intraretinal cysts over chorioretinal scarring
She had a recurrence of anterior uveitis in left eye which was treated with topical steroids. Due to ongoing uveitis and recurrent bilateral CME (cystoid macular edema), she warranted advancement of her systemic immunomodulatory therapy and Humira was initiated. The patient also received an OZURDEX® (dexamethasone intravitreal implant) in the left eye which led to almost complete resolution of IRF (intraretinal fluid) in the left eye.
It was hypothesized that some of the IRF might be non-modifiable due to degenerative cysts over areas of atrophy with ERM (epiretinal membrane).
Over subsequent visits, her visual acuity in the left eye worsened from her baseline of 20/80 OS to 20/150 OS (cc). Prior to OZURDEX® injection, her exam was notable for a 1+ noncentral posterior subcapsular cataract (PSC) in the left eye. Over the next year, this progressed to a 2+ central PSC with anterior cortical changes.
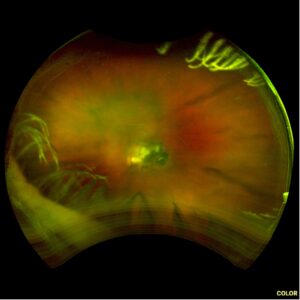
Figure 3. Left eye fundus photo 10 months after dexamethasone intravitreal implant.
While previous retinal findings are still visible, note the central PSC obstructing the visual axis and additional anterior cortical spoking.
After ruling out macular etiologies of her visual decline (macula OCT stable from previous), she underwent cataract surgery with intraocular lens placement in the left eye, which resulted in an improved VA from 20/150 (mr) to 20/80 OS sc on post-op day 1.
Discussion:
Cataract formation can be accelerated due to myriad causes, including inflammatory processes like uveitis (specifically ocular sarcoidosis in the above patient’s case). Both the disease (uveitis) as well as a mainstay of its treatment (steroids) lead to cataract formation in patients with uveitis. Because the lens material is a crystalline structure that is avascular, nutrition and maintenance of the lens are derived from intraocular fluid contents. It follows that intraocular inflammation, and inflammatory cytokines, disrupt the metabolism of the lens through diffusion, particularly posteriorly. This is largely due to the lack of endothelial support at the back of the lens. Cataracts in eyes with uveitis require a different set of considerations when approaching a surgical decision.
Diagnosis:
The most common symptoms of age-related cataracts are decreasing visual acuity/clarity both at distance and near, and glare and halos, particularly at night; however, diagnosis of a uveitic cataract must be secondary to a confirmed case of uveitis and is more likely to present with a PSC that creates visually significant changes. Uveitic cataracts may be surgically addressed if they obscure posterior segment pathology and preclude appropriate monitoring of disease activity or less urgently when interfering with the patient’s visual function.
Management/Considerations:
When approaching the uveitic cataract, considerations must be made to account for infectious versus inflammatory uveitis. In cases of uveitis due to viral etiologies, such as HSV or VZV anterior uveitis or acute retinal necrosis, it is prudent to increase systemic antivirals to therapeutic levels in the peri-operative period. In the case of sarcoid uveitis and other chronic ocular inflammatory diseases, having an eye without active inflammation for 3 months is recommended prior to cataract surgery. This may be achieved with an appropriate immunomodulatory regimen.
Inflammation control:
To mitigate the risk for inflammatory flares and complications both pre- and postoperatively, steroids are considered standard of care. Topical eye drops (prednisolone acetate 1%), oral prednisone and periocular or intraocular steroids are often used individually and in combination to maximally decrease the risk of a uveitis flare in the perioperative period.
Surgical control/challenges:
Both the size of the surgical incision and the capsulorhexis should be of sufficient length/diameter to prevent iris prolapse and decrease the risk of capsular phimosis and posterior synechiae respectively. An in-the-bag lens placement has been highly preferred as it reduces the chances of subsequent inflammation, although ongoing research suggests that sulcus placement might have advantages. Small pupils, anterior or posterior synechiae, and zonular dehiscence, which can all be a result of uveitis, increase the risk of zonular dehiscence, anterior chamber hemorrhage and pigment dispersion and must be approached with care. Additionally, the anterior capsule can often be fibrotic and can require additional manipulation during capsulorhexis and cause tension on the zonules.
Postoperative considerations:
In addition to inflammation control, due to the use of steroids coupled with an intraocular surgery, intraocular pressure should be monitored closely for both pressure spikes and low pressures that may be concerning for ciliary body failure, ciliary effusion, cyclitic membranes or early phthisis. Other complications in the post-operative period can include the formation of a posterior capsular opacity (PCO), cystoid macular edema (CME), and epiretinal membrane formation (ERM), among others.
Format: Case Report
References:
- Shaw E, Patel BC. Complicated Cataract. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572139/
- Liu YC, Wilkins M, Kim T, Malyugin B, Mehta JS. Cataracts. Lancet. 2017 Aug 5;390(10094):600-612. doi: 10.1016/S0140-6736(17)30544-5. Epub 2017 Feb 25. PMID: 28242111.
- Alekseev BN, Sibai SA. Opredelenie termina “oslozhnennye katarakty” [Definition of the term “complicated cataracts”]. Vestn Oftalmol. 1996 Sep-Oct;112(4):26-7. Russian. PMID: 9019908.
- Avetisov SE, Razumova IY, Avetisov KS. Rezul’taty khirurgicheskogo lecheniya oslozhnennoi uveal’noi katarakty [Results of surgical treatment of complicated uveal cataract]. Vestn Oftalmol. 2020;136(5. Vyp. 2):209-213. Russian. doi: 10.17116/oftalma2020136052209. PMID: 33063966.
- Avetisov SE, Razumova IY, Avetisov KS. Rezul’taty khirurgicheskogo lecheniya oslozhnennoi uveal’noi katarakty [Results of surgical treatment of complicated uveal cataract]. Vestn Oftalmol. 2020;136(5. Vyp. 2):209-213. Russian. doi: 10.17116/oftalma2020136052209. PMID: 33063966.
Faculty Approval by: Marissa Larochelle, MD
Copyright statement: Copyright Amanda Wade, Marissa Larochelle, ©2024. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/