Optic Atrophy
Home / Basic Ophthalmology Review / Optic Nerve
Title: Optic Atrophy
Author: Sean Collon, MSIV, Vanderbilt University School of Medicine
Photographer: James Gilman, CRA, FOPS
Date: 08/07/2017
Keywords/Main Subjects: Optic atrophy; glaucoma; optic neuropathy; hereditary optic neuropathy
CORE Category: Med Student Outline; Anatomical Approach to Eye Disease; Optic Nerve; Optic Atrophy
Diagnosis: None
Description:
Introduction
Optic atrophy is a term that describes the finding of a pale optic nerve head, indicating the death of retinal ganglion cells due to injury at some point along their course from the retina to the lateral geniculate nucleus. It represents the end stage of an underlying pathologic process, typically developing 4-6 weeks after onset of symptoms in most optic neuropathies, even after recovery of some or all vision. Because there is currently no way of regenerating retinal ganglion cells in humans, vision loss due to optic atrophy is permanent.
Differential Diagnosis
Optic atrophy is diagnosed by the visualization of a pale optic disc on fundoscopic evaluation and may be accompanied by findings suggestive of the underlying etiology, such as cupping or papilledema. On the other hand, the classic triad of vision loss, relative afferent pupillary defect, and pale disc yields a vast differential that includes:
- Inflammation/Infiltrative process: sarcoid, lupus, multiple sclerosis, lymphoma/leukemia
- Infection: herpes, TB, syphilis
- Ischemia: arteritic versus non-arteritic ischemic optic neuropathy, diabetes
- Compression:
- Intraocular: glaucoma
- Intraorbital: tumor, optic nerve glioma, thyroid eye disease
- Extraorbital: meningioma or some other intracranial tumor or mass
- Toxic/Metabolic Causes: B12 deficiency, medications (e.g. ethambutol, amiodarone), methanol ingestion, heavy metals
- Trauma: traumatic optic neuropathy
- Hereditary Causes: Autosomal dominant optic atrophy, Leber’s hereditary optic neuropathy
Management
The workup for a patient with optic atrophy has two primary goals: to assess the extent of damage/ remaining visual potential and to identify and remove the underlying etiology to preserve remaining vision.
Optic nerve function can be assessed with visual acuity, color vision testing, and quantitative perimetry. Optical coherence tomography (OCT) can be used to establish and monitor retinal nerve fiber layer (RNFL) thickness, but can be confounding in cases of optic atrophy due to papilledema, where RNFL thinning may mimic resolution of papilledema. Finally, fundus photography can be helpful in documenting the extent of atrophy and monitor changes in the pattern of atrophy over time.
Patients will often present with signs or symptoms that suggest a specific etiology, and testing should be tailored accordingly. For the patient with otherwise undifferentiated optic atrophy, initial workup should include MRI of the brain and orbits with gadolinium contrast, blood work including CBC, CMP, folate, B12, heavy metals and inflammatory markers such as ESR, CRP in the elderly. If no cause is identified and the patient remains stable symptomatically, observation may be reasonable. However, if symptoms worsen or recur, further workup is indicated.
Images or video:

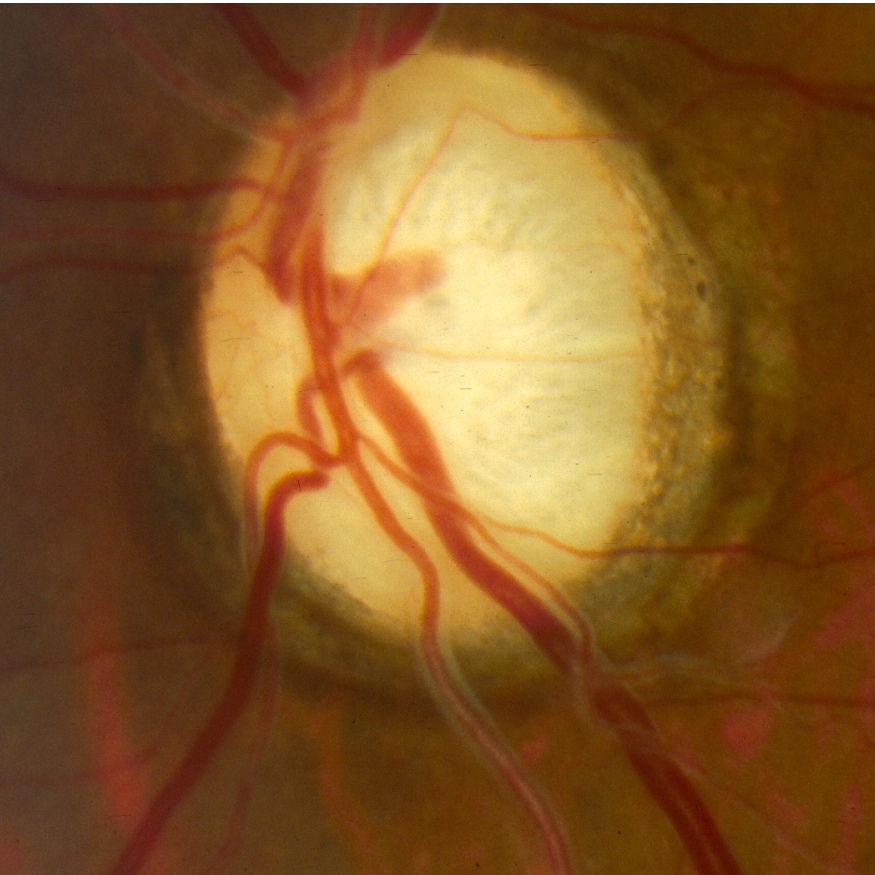
Color fundus photo of the right eye showing subtle temporal optic atrophy—the temporal part of the disc here is on the observer’s left.
Summary of the Case: Optic atrophy is the finding of a pale optic nerve head, which indicates the death of retinal ganglion cells from any of a number of causes, including inflammation, infection, ischemia, compression, toxicity, trauma, or hereditary conditions. Management consists of identifying and treating the cause of optic nerve damage and preserving what vision remains.
References:
- Osaguona VB. Differential diagnoses of the pale/white/atrophic disc. Community Eye Health. 2016;29(96):71-74.
- Girkin CA. 2016-2017 Basic Clinical Science Course, Section 05, Neuro-Ophalmology. San Francisco, CA: American Academy of Ophthalmology, 2017. Web. 17 Aug 2018.
Faculty Approval by: Griffin Jardine, MD
Copyright Sean Collon, ©2018. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/
Identifier: Moran_CORE_25534