Ultrasound of a Patient with Terson Syndrome Secondary to a Gunshot Wound
Retina and Vitreous / Other Retinal Vascular Diseases
Title: Ultrasound of a Patient with Terson Syndrome Secondary to a Gunshot Wound
Author: Mark Parsons, MS4
Photographer: Roger Harrie, MD
Date: July 2, 2024
Secondary CORE Category: Retina and Vitreous / Posterior Segment Manifestations of Trauma; Ultrasound
Keywords/Main Subjects: Terson syndrome, intracranial hemorrhage, intraocular hemorrhage, trauma, ultrasound
Diagnosis: Terson Syndrome
Description of Case:
The images shown are from 23 year-old male who originally presented to the emergency department following a gunshot wound to the head. At the time, he underwent emergent hemicraniectomy for resection of a right temporal lobe hematoma, with concomitant subarachnoid and subdural hemorrhages noted on imaging. He experienced remarkable cognitive recovery and was discharged to a rehabilitation facility 18 days after presentation. Upon arrival at the new facility, ophthalmology was consulted for evaluation of visual complaints. The patient reported limited vision, ophthalmoplegia, and ptosis in the right eye (OD) that had been present since first awakening in the hospital. Evaluation was concerning for orbital apex syndrome and Terson syndrome, and B scan (as shown above) revealed vitreous hemorrhage in addition to focal subretinal, subhyaloid, or sub-internal limiting membrane (sub-ILM) hemorrhage. Vitrectomy with internal limiting membrane (ILM) peel was performed OD for removal of vitreous hemorrhage and what proved to be sub-ILM hemorrhage. At postoperative day 1, visual acuity (VA) was counting fingers at two feet. VA improved to 20/40 by postoperative day 9, and to 20/20 by postoperative week 6.
Defined most broadly, Terson syndrome is any intraocular hemorrhage in the setting of intracranial hemorrhage or an acute increase in intracranial pressure. The pathogenesis is not fully agreed upon, but a leading proposed mechanism is that rapid increase in intracranial pressure leads to an efflux of cerebrospinal fluid down the optic nerve sheath, compressing the central retinal vein and causing rupture of small retinal vessels.
Symptoms of Terson syndrome vary, with some patients being asymptomatic and others reporting loss of vision. Additionally, some may be unable to communicate their symptoms due to neurologic compromise. Fundoscopy may reveal varying forms of intraocular hemorrhage, including vitreous, subhyaloid, sub-ILM, intraretinal, or subretinal hemorrhages, either unilaterally or bilaterally. A classic “double ring sign” is sometimes present due to the presence of overlying subhyaloid and sub-ILM hemorrhages. If visualization is obscured or mydriasis is contraindicated, ultrasound or CT may be useful for diagnosis. Ultrasound is particularly helpful in cases of vitreous or preretinal hemorrhage. Most cases of Terson syndrome develop soon after the intracranial insult, but delayed presentations have been described. From an ophthalmic perspective, Terson syndrome may be managed via observation or vitrectomy. In cases of sub-ILM hemorrhage, an ILM peel may also be performed intraoperatively.
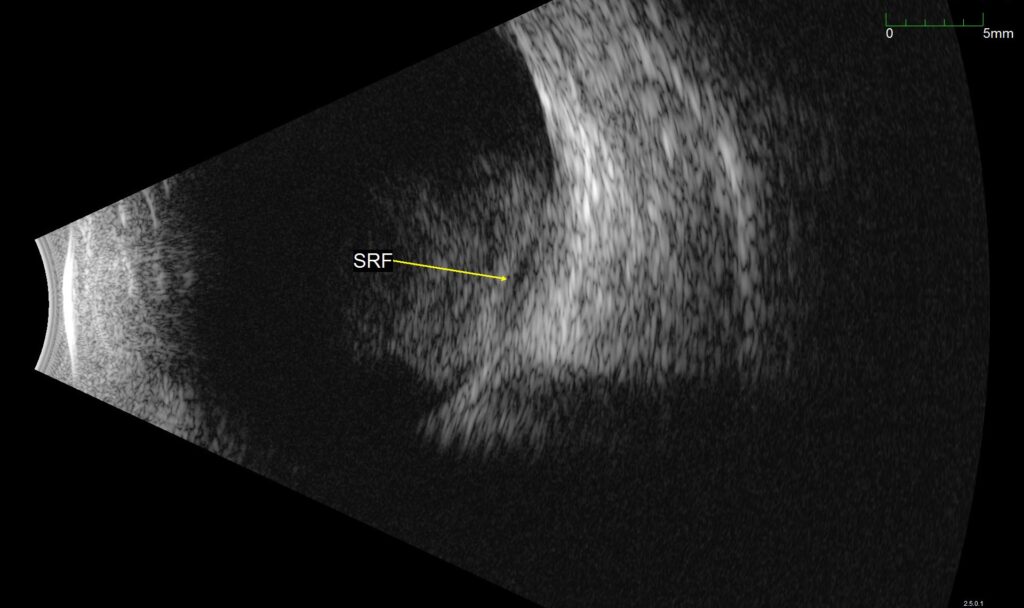
Figure 1. B-scan ultrasound of the affected eye. Vitreous hemorrhage can be seen over the posterior pole, with a second underlying hemorrhage, labeled SRF in the image. This was found to represent a sub-ILM hemorrhage intraoperatively.
Summary of the Case: A 23 year-old male was evaluated for Terson syndrome after being hospitalized for intracranial hemorrhages secondary to a gunshot wound to the head. B-scan revealed vitreous hemorrhage in the right eye with an additional second hemorrhage, which proved to be a sub-ILM hemorrhage. He underwent vitrectomy with ILM peel, and VA improved from counting fingers to 20/20 by postoperative week 6.
References:
- Ko F, Knox DL. The ocular pathology of Terson’s syndrome. Ophthalmology. 2010;117(7):1423-9.e2. doi:10.1016/j.ophtha.2009.11.028
- Reale C, Brigandì A, Gorgoglione N, Laganà A, Girlanda P. Terson’s syndrome. Practical Neurology. 2020;20(2):163-164. doi:10.1136/practneurol-2019-002326
- Stevanovic M, Eliott D. Terson Syndrome: A Review of the Literature. International Ophthalmology Clinics. 2024;64(2):89. doi:10.1097/IIO.0000000000000502
- Terson Syndrome: Don’t Let It Go Unrecognized. American Academy of Ophthalmology. Published October 31, 2018. Accessed June 30, 2024. https://www.aao.org/eyenet/article/terson-syndrome-dont-let-it-go-unrecognized
Faculty Approval by: Akbar Shakoor, MD
Copyright statement: Copyright Mark Parsons, ©2024. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/



