Confrontation Visual Fields
Home / Allied Ophthalmic Training Program
 Loading...
Loading...
Title: Allied Ophthalmic Training: Confrontation Visual Fields
Author (s): Kathryn Durnford, MS3, University of Utah; Sophia Fang, MD, Fellow, Moran Eye Center
Photographer: Kathryn Durnford (images of VF testing)
Date: 5/26/20
Keywords/Main Subjects: Confrontation visual fields, ophthalmic training, five vital signs of ophthalmology
Diagnosis: n/a
Description of Case: Information on performing confrontation visual fields for ophthalmic professionals of all skill levels. The information included is relevant to those who are learning these skills for the first time or for experienced healthcare professionals looking to refine their skills.
Summary of the Case: Information about the definition of a visual field and how to properly assess the visual field through confrontation is contained. Examples on how to correctly assess the visual field are shown as well.
Format: PowerPoint (main); PDF (supplemental)
References: Stein, H., Stein, R., & Freeman, M. (2018). The ophthalmic assistant. [s.l]: Elsevier.
Faculty Approval by: Griffin Jardine, MD; Sophia Fang, MD
Copyright: Kathryn Durnford, ©2020. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/
Identifier: Moran_CORE_28368
Purpose of Dilation/ B-Scan
 Loading...
Loading...
Removal of Superficial Corneal Foreign Bodies
Home / Basic Ophthalmology Review / Removal of superficial foreign bodies
Title: Removal of Superficial Corneal Foreign Bodies
Author: Austin D. Bohner, MS3 University of Utah
Photographer: James Gilman, CRA, FOPS; Ethan Peterson; Melissa Chandler; Mary Mayfield
Date: 01/08/19
Keywords/Main Subjects: Cornea, Foreign Body
Diagnosis: Superficial Corneal Foreign Body
Images:

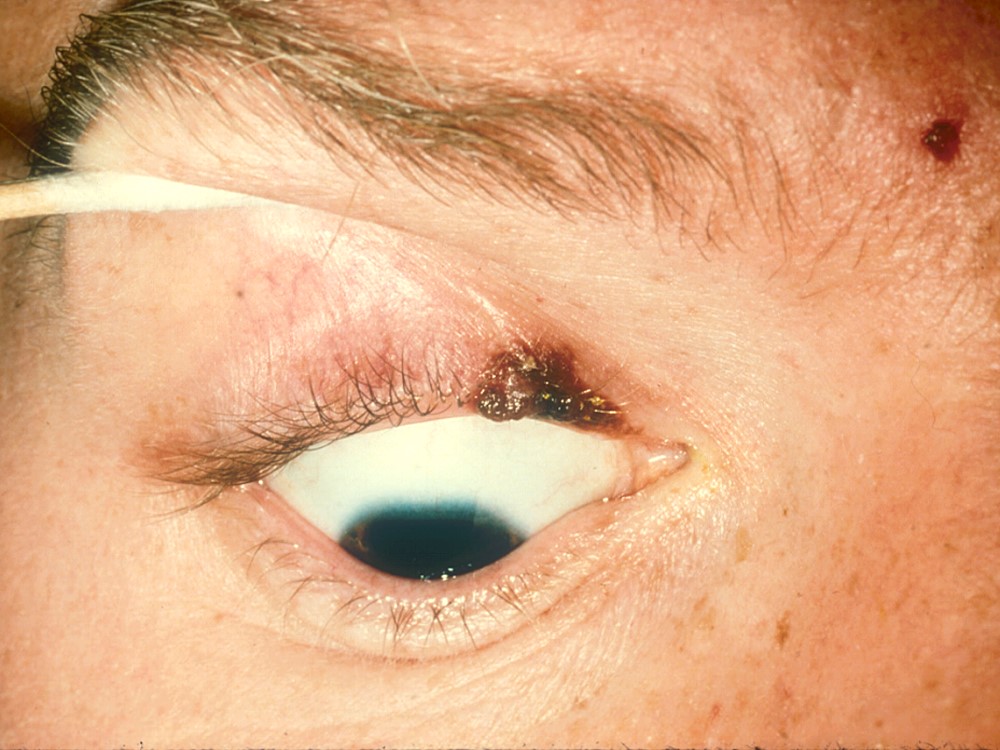
Figure 1: Deep corneal injury with penetration into the anterior chamber. Also observe dense cataract and iris distortion.
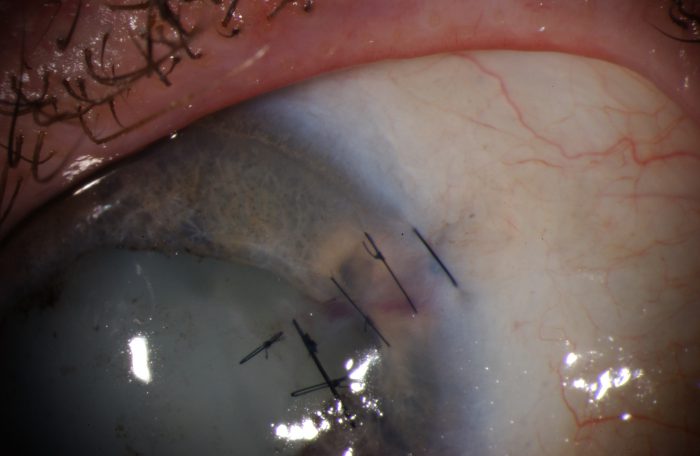
Figure 2. Post-removal and repair of deep penetrating corneal foreign body with anterior chamber perforation. The repair was performed in a sterile operating room under general anesthesia. Simple interrupted sutures using 10-0 monofilament were placed to close globe penetration with the goal of preventing leak and anterior chamber collapse.
Clinical Identification and Management:
Superficial corneal foreign bodies (SCFB) are easily seen and usually can be removed in clinic or the ED with minimal or no long term complications.1 SCFB are best identified through slit lamp microscopy. The source of the SCFB is often revealed through patient history and allows clinicians to assess the risk of infection after removal of the material.1 Metals are common SCFB culprits and are often seen in malleolus workers at risk for high-speed metallic particles lodging in the eye.2 Activities with the highest associated risk of SCFB include high-speed metal grinding and metal-on-metal hammering.2 It is recommended that workers engaging in these risky activities utilize eye glass protection for SCFB prevention.
Trained clinicians can easily remove SCFB. Before attempting to remove a SCFB, however, the clinician should first assess the depth of penetration and rule out a ruptured globe or intraocular foreign body.3 Particles penetrating beyond bowman’s layer will result in some degree of corneal scarring. Deep corneal infiltration or penetration of the anterior chamber (Figure 1) may warrant utilization of a different removal technique. In the case of a full thickness corneal laceration the eye should be shielded and no manipulation of the cornea attempted until the patient paralyzed and sedated under anesthesia, for risk of expulsing intraocular contents. Full thickness corneal lacerations may require the use of corneal sutures in order to secure the globe and prevent anterior chamber collapse (Figure 2.)
When treating a superficially lodged corneal foreign body, adequate topical anesthesia with ophthalmic eye drops (such as proparacaine) is imperative. Removal of SCFB should be performed using a slit lamp for visualization. Retoillumination with slit lamp microscopy can be used to visualize a small corneal foreign body (Figure 3.) The patient should be instructed to fix their gaze straight ahead and focus on a specific target, such as a far-away point or the clinician’s ear. The patient’s forehead should be pressed completely against the forehead plate of the slit lamp to optimize stabilization during SCFB removal. During the procedure, it is recommended to adjust the light source to being bright enough to clearly visual the cornea but dim enough to be tolerable to the patient. Removal of the SCFB can be achieved using a 25-30 gauge, sterile, disposable, hypodermic needle. The clinician should operate the slit lamp with one hand, using the other hand to hold the needle and manipulate the eyelid if necessary. When using the needle, always approach the cornea in a tangential plane and never in perpendicular alignment, as it is likely to intensify patient anxiety and increase the risk of inadvertent corneal perforation. In the tangential plane, with the bevel facing away from the corneal, the SCFB can be gently scraped away. A rust ring is commonly seen after removal of iron-containing SCFBs. The remaining rust ring can be carefully scrapped away with any additional ring remains self-resolving by reabsorption over time.
Removal can also be achieved through use of a battery-powered dental burr, similar to a Dremel drill (Figures 4-6). The battery-powered dental burr can be used as a complimentary removal tool to the hypodermic needle. In some instances the burr may be used in lieu of a hypodermic needle, depending on clinician preference. Prior to use, the burr tip should be sterilized in a standard fashion. Similar to the hypodermal needle, burr tip should be used in a tangential corneal plane.
Topical antibiotics are recommended for all patients following removal of the SCFB.2,3 Furthermore, dilating eye drops (such as 1% cyclopentolate or atropine) and the use of a contact bandage lens can be useful for some patients. Patients should be monitored for signs of infection with close follow-up.
Faculty Approval by: Griffin Jardine, MD
References:
- Wipperman JL, Dorsch JN. Evaluation and management of corneal abrasions. Am Fam Physician. 2013;87(2):114-120.
- DeBroff BM, Donahue SP, Caputo BJ, Azar MJ, Kowalski RP, Karenchak LM. Clinical characteristics of corneal foreign bodies and their associated culture results. CLAO J. 1994;20(2):128-130.
- Ophthalmology AAo. 2015-2016 BCSC (Basic and Clinical Science Course). In: External Eye Disease and the Cornea. American Academy of Ophthalmology; 2015:355-356.
Identifier: Moran_CORE_26928
Copyright statement: Copyright ©2019. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/
Conjunctivitis
Home / Basic Ophthalmology Review / Conjunctiva / Sclera
Title: Conjunctivitis
Authors: Trey Winter, 1st Year Medical Student, University of Utah; Mike Murri, MD, University of Utah Moran Eye Center
Photographer: James Gilman, CRA, FOPS
Images:

Figure 1: External photograph demonstrating allergic conjunctivitis. Note the injected conjunctival vessels and associate nodules at the limbus.

Figure 2: A case of vernal conjunctivitis showing the typical elevated, gelatinous conjunctival nodules at the limbus.

Figure 3: A case of chronic, untreated chlamydial conjunctivitis with significant scarring found on the undersurface of the upper eyelid, or the palpebral conjunctiva. There is significant scarring which is quite specific to this entity but typically only in cases with delayed treatment, most often seen in the developing world.
Definition
Conjunctivitis is the inflammation of the conjunctiva. The conjunctiva is the mucous membrane that lines the inner eyelid and covers the sclera up to the cornea. The conjunctiva can be divided into two anatomical can also be divided into two areas: the bulbar conjunctiva, which covers the actual eye; and the palpebral conjunctiva, which extends onto the undersurface of the eyelids. The “red eye” or “pink eye” appearance of the conjunctiva is secondary to inflammation which can be caused by hyperemia (increased blood flow) and increased diameter of conjunctival blood vessels which causes edema. Inflammation can also cause an acute generalized hyperplasia or lymphocyte aggregation in the lymphoid layer of the conjunctiva.
Conjunctivitis is divided into two broad categories: infectious and non-infections. Infectious conjunctivitis can be subclassified as bacterial or viral. Non-infectious conjunctivitis can be subclassified as allergic or non-allergic.
All types of conjunctivitis typically present with reddening of the conjunctiva. Additionally, inflammation and epiphora (watery eye) are common presentation signs. Conjunctivitis does not typically impair vision and pupils should still be reactive to light.
Infectious Conjunctivitis
Viral
Viral conjunctivitis is often accompanied by signs of a viral infection in the upper respiratory tract. Viral conjunctivitis is extremely contagious and is spread by contact with secretions from those infected, fomites contaminated with the virus, or from public areas such as swimming pools. Adenovirus is the most common viral infectious agent. Other viral agents causing conjunctivitis include Herpes Simplex Virus 1 and enteroviruses.
Viral infectious conjunctivitis typically presents with upper respiratory tract symptoms such as a runny nose or sore throat. Lymph nodes are often enlarged on the same side of the affected eye upon physical exam. The eye is usually excessively watery accompanied by irritation and pruritis. Patients may complain of a sandy or gritty feeling in the infected eye, and the appearance of the eye is usually diffusely pink. Viral infections of the conjunctiva usually begin unilaterally, but often will spread through contact to eventually infect both eyes. The symptoms can last a few weeks and don’t respond to antibiotic eye drops.
Bacterial
Bacterial conjunctivitis is commonly caused by Staphylococcus aureus, Streptococcus pneumonia, Haemophilus influenza, and Moraxella catarrhalis. These organisms can spread from the nasal and sinus mucosa or from another affected individual. Adult bacterial conjunctivitis is typically caused by Staphylococcus aureus while children commonly contract the other three pathogens listed above. An extreme case of acute bacterial conjunctivitis caused by the sexually transmitted Neisseria gonorrhoeae can lead to blindness through rapid spread to the corneal surface and typically occurs very rapidly. It is transmitted from genitals to the hands and finally to the eyes. Chlamydia trachoma presents in a similar manner to Neisseria but the development is slow and insidious (see Image 3).
Unlike viral conjunctivitis, bacterial conjunctivitis presents with a sticky, purulent discharge. This discharge can be yellow, white or green in color. Patients with conjunctivitis of all types can present with a crusted, closed eye in the morning from discharge, however with bacterial conjunctivitis, thick purulent discharge will persist throughout the day. In addition, patients with bacterial conjunctivitis often do not experience pruritis. Like viral conjunctivitis, bacterial conjunctivitis initially presents unilaterally, eventually spreading to the other eye.
Other infectious causes
Other less-common causes of conjunctivitis beyond scope of this article but that can be considered are fungal, parasitic, and rickettsial pathogens.
Non-Infectious Conjunctivitis
Allergic
Allergic conjunctivitis is a type-1 hypersensitivity reaction caused by airborne or other allergens. The allergens cause the degranulation of mast cells and release of histamine and other factors causing swelling and redness of the conjunctiva. This swelling can present on the palpebral conjunctiva as a cobblestone appearance with central blood vessels (papillae, see Image 4 for a dramatic case).
Allergic conjunctivitis presents similarly to viral conjunctivitis with a few key differences. Like viral conjunctivitis, allergic conjunctivitis presents with injection (redness), a watery discharge, and itching. A key distinguishing factor is that allergic conjunctivitis more commonly presents bilaterally and often has more lid irritation. The itching in allergic conjunctivitis is constant and not accompanied by the additional description of sandy or gritty. Patients may develop elevated conjunctival nodules at the limbus with chronic, allergic conjunctivitis (see Images 1 and 2). A history of asthma, exczema, or specific allergies or hay fever are key factors in suspecting allergic conjunctivitis, as well as new pets, makeup, eye drops, creams or lotions.
Non-allergic
Non-allergic conjunctivitis it classically caused by a chemical or physical problem. Chemicals splashed in the eye may cause mucus formation and redness, but will typically resolve within 24 hours. The two common factors relating to physical problems are dryness or a foreign body. The most common foreign body-induced non-allergic conjunctivitis are contacts. A reaction to contacts is most commonly seen in those who have poor contact-lens hygiene (sleeping in contacts, extended use of contacts, improper storage, etc.).
Non-allergic conjunctivitis has a variable presentation depending on the cause. Discharge is more commonly mucus as opposed to pus. Most of these cases resolve after around 24 hours or after removal of the foreign body.
Complications
Conjunctivitis does not regularly cause complications with the exception of the sexually transmitted bacterial infections. Complications are more common in those that are immunocompromised.
Complications from conjunctivitis (in order of most common to least common) include: keratitis (infection of the cornea), cellulitis, otitis media, genital coinfection, bacteremia and meningitis.
Differential Diagnosis
The differential diagnosis for conjunctivitis is broad and includes many conditions causing a red eye. Conditions include, but are not limited to: keratitis, angle-closure glaucoma, iritis, corneal abrasion, subconjunctival hemorrhage, pinguecula, blepharitis and poor contact lenses fit.
Diagnosis
It is important to make an accurate diagnosis of conjunctivitis and to educate patients on the etiology of their disease. Many patients with conjunctivitis will assume that there is a bacterial cause and desire antibiotics. It is important to take a detailed history and perform a physical exam including signs of upper respiratory infection and lymph node examination. Diagnosis can be made based on the presentations detailed above. On physical examination of conjunctivitis, the red reflex and visual acuity should be intact. Presentation of visual problems in addition to the physical findings indicate another condition.
Typically, cultures are not required for diagnosis. Information in the history and on physical examination can assist in diagnosis of the type of conjunctivitis. Persistent cases that do not respond to treatment may necessitate a bacterial and fungal culture. Rapid adenovirus tests exist that can be used to definitively diagnose an adenoviral conjunctivitis, but this is usually unnecessary.
Physical examination is especially important in patients who use contact lenses, as the reddening of the eye can be caused by poorly fitting contacts or poor contact lens hygiene. Removal of the contacts for a period may reveal if contacts are the cause of the injection.
Management/Treatment
Conjunctivitis is usually self-limiting and treatment reduces symptoms, but does not speed duration of the illness. For bacterial conjunctivitis, antibacterial eye drops are not always necessary but may be prescribed to decrease the severity of the infection. In areas with high risk of contagion such as schools and daycare centers, patients must often be treated for 24 hours before they can return. In these cases a topical antibiotic that is inexpensive and nontoxic may be given. The treatment of bacterial conjunctivitis is erythromycin ointment or trimethoprim-polymixin eye drops.
Viral conjunctivitis can be treated with antihistamines or lubricating agents to provide relief of the symptoms and inflammation. Notably these do not actually treat the viral root cause. The same treatment is administered for patients with non-allergic conjunctivitis.
Allergic conjunctivitis can be treated with antihistamines, artificial tears, and if known, avoiding the agents that cause the allergic reaction. A patch test can be performed for patients with severe allergies. In all cases of conjunctivitis, patients should be advised to avoid contact lens use, refrain from rubbing the eyes, and wash hands frequently.
References:
Azari, AA; Barney, NP (23 October 2013). “Conjunctivitis: a systematic review of diagnosis and treatment”. JAMA. 310 (16): 1721–9.
Fitch CP, Rapoza PA, Owens S, et al. Epidemiology and diagnosis of acute conjunctivitis at an inner-city hospital. Ophthalmology 1989; 96:1215.
Friedlaender MH. A review of the causes and treatment of bacterial and allergic conjunctivitis. Clinical Therapy 1995; 17:800.
Gigliotti F, Williams WT, Hayden FG, et al. Etiology of acute conjunctivitis in children. Journal of Pediatric Medicine 1981; 98:531.
Wan WL, Farkas GC, May WN, Robin JB. The clinical characteristics and course of adult gonococcal conjunctivitis. American Journal of Ophthalmology 1986; 102:575.
Weiss A, Brinser JH, Nazar-Stewart V. Acute conjunctivitis in childhood. Journal of Pediatric Medicine 1993; 122:10.
Faculty Approval by: Griffin Jardine, MD
Identifier: Moran_CORE_26899
Copyright statement: Copyright ©2019. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/
Ptosis
Home / Basic Ophthalmology Review / Lids/Lashes
Title: Ptosis
Author: Celestine Gregerson, MSIII University of Utah; Tom Dowdle, Matriculated Medical Student, University of Utah
Photographer: James Gilman, CRA, FOPS
Images:

Figure 2: Asymmetric bilateral ptosis, more severe on the left. Obstruction of the pupil is present on both sides, resulting in significant bilateral visual field impairment

Figure 3: Dermatochalasis causing pseudoptosis, or drooping of the skin above the eyelids resulting in the appearance of ptosis.
Overview:
Blepharoptosis or ptosis refers to the drooping of the upper eyelid with an associated decrease in the vertical palpebral fissure, or the distance between the upper eyelid and lower eyelid.1,2 Ptosis occurs due to an abnormality in the structures that elevate the upper eyelid. In severe cases, ptosis can obstruct the pupil and cause visual field impairment. Etiologies include both congenital and acquired causes. Acquired causes include aponeurotic, neurogenic (the potentially emergent causes), and mechanical.
Classification & Etiology:
- Congenital: The most common cause of ptosis in children is due to the improper development of the levator palpebrae superioris muscle (levator), which functions to elevate the upper eyelid1,3. This is apparent on exam because there is no lid crease, which is where the levator normally inserts. Congenital ptosis is considered an emergency if the eyelid is obstructing vision because it can result in irreversible amblyopia or even vision loss if left untreated.
- Aponeurotic: The most common cause of ptosis in adults is due to weakening or disinsertion of the levator aponeurosis, the collagenous insertion of the levator on the eyelid. It may develop with aging, contact lens wear, chronic eyelid rubbing, or eye surgery.4-6 Aponeurotic ptosis typically is non-emergent and gradual in onset, but can cause significant upper visual field impairment.
- Neurogenic: Neurogenic ptosis is a potential emergency, especially when sudden onset. There are two especially concerning neurogenic causes: Horner’s syndrome and a cranial nerve III palsy. Myasthenia gravis is a less common cause of neurogenic ptosis.
- Horner’s Syndrome: This classically presents as a triad of findings due to disruption of the sympathetic innervation to the eye/face: ptosis, miosis (small pupil), and anhidrosis (absence of normal flushing/sweating). The ptosis is due to impaired innervation of the Müller’s or superior tarsal muscle, which is supplemental to the levator in elevating the eyelid. When sudden onset, it can be secondary to a carotid dissection, which warrants emergent referral to an Emergency Department for evaluation. In children, this can be secondary to a neuroblastoma compressing the sympathetic chain.
- Cranial Nerve III Palsy: Damage or disruption of this cranial nerve causes eyelid drooping because it innervates the levator. Typically, the ptosis is unilateral and the affected eye will present in a down-and-out position with a blown pupil1. The concerning etiology in these cases is an aneurysm or tumor compressing the nerve, and should be emergently referred for evaluation.
- Myasthenia Gravis: Fatigable unilateral or bilateral ptosis, as well diplopia or weakness of the orbicularis oculi often results from this autoimmune disorder. Ptosis seen in myasthenia gravis patients can be differentiated from other causes of ptosis by its temporary resolution with an ice-pack or an acetylcholine esterase inhibitor.1
- Mechanical/Traumatic Ptosis: Mechanical ptosis is a gravity-related drooping that occurs when there is edema, ecchymosis, or a mass of the upper eyelid that causes the lid to droop down. Trauma to the orbit can cause mechanical ptosis. However, trauma can also cause muscle or nerve damage resulting in persistent ptosis that does not resolve as local tissues heal.
- Other causes:
- Muscular disorders such as mitochondrial myopathies, myotonic dystrophy, and oculopharyngeal muscular dystrophy
- Neurotoxic causes such as botulinism or envenomation
Ptosis should not be confused with pseudoptosis, which is the perceived appearance of a dropping eyelid due to abnormalities of the globe or surrounding skin1. Pseudoptosis most commonly occurs as a result of dermatocholasis, the process in which the skin above the eyelid becomes less elastic and droops below the eyelashes7. Other causes of pseudoptosis include severe enophthalmos, ipsilateral hypotropia, brow ptosis, and contralateral lid retraction giving the impression of relative ptosis of the opposite lid.7
Evaluation:
Obtaining a thorough history, including any associated events or symptoms concerning for thyroid pathology or neurological abnormalities, is a first and critical step of ptosis evaluation7. The exam includes measuring:
- The function of the levator and superior tarsal muscles: how well the eyelid elevates when the patient is instructed to look up
- Comparing the distance between the eyelid and the center of the pupil between the two eyes in primary gaze
- Noting the presence or absence of an upper eyelid fold
- Noting any adaptations on the part of the patient:chin up posture or voluntary elevation of brows1,2,7
Management:
After the emergent causes of ptosis have been ruled out or addressed, candidacy for nonsurgical therapies in patients with myasthenia gravis or Horner syndrome can be considered. Eyelid crutches can be attached to eyeglasses for temporary relief in some patients. Surgery is the definitive corrective measure for patients with ptosis causing superior visual field loss.1,2,7 A variety of surgical approaches can be taken, including resection of the levator aponeurosis or eyelid suspension.2,7,8
Faculty Review: Griffin Jardine, MD
References:
- Patel K, Carballo S, Thompson L. Ptosis. Disease-a-Month (Clinical Issues in Ophthalmology – Part II). 2017; 63(3):74-79.
- Sudhaker P, Vu Q, Kosoko-Lasaki O, Palmer M. Upper eyelid ptosis revisited. American Journal of Clinical Medicine. 2009; 6 (3):5-14.
- Baldwin HC, Manners RM. Congenital Blepharoptosis: A Literature Review of the Histology of Levator Palpebrae Superioris Muscle. Ophthalmic Plastic and Reconstructive Surgery. 2002; 18 (4):301-307.
- Kersten RC, de Conciliis C, Kulwin DR. Acquired Ptosis in the Young and Middle-aged Adult Population. Ophthalmology. 1995; 102 (6):924-928.
- Mehat MS, Sood V, Madge S. Blepharoptosis Following Anterior Segment Surgery: a New Theory for an Old Problem. Orbit. 2012; 31 (4):274-278.
- Fujiwara T, Matsuo K, Kondoh S, Yuzuriha S. Etiology and Pathogenesis of Aponeurotic Blepharoptosis. Annals of Plastic Surgery. 2001; 46 (10):29-35.
- Fausett, BV, Nerad JA. Upper Eyelid Ptosis and Retraction. Diseases and Disorders of the Orbit and Ocular Adnexa. 2017; Ch 28: 525-539.
- Frueh BR, Musch DC, McDonald HMB. Efficacy and efficiency of a small-incision, minimal dissection procedure versus a traditional approach for correcting aponeurotic ptosis. Ophthalmology. 2004; 111(12):2158-2163.
Identifier: Moran_CORE_26610
Disc Edema
Home / Basic Ophthalmology Review / Optic Nerve
Title: Disc Edema
Author: Cole Swiston, 4th year medical student, University of Wisconsin School of Medicine and Public Health; Trey Winter, 1st Year Medical Student, University of Utah
Photographers: Danielle Princiotta, Becky Weeks
Figure 1. Bilateral optic disc edema (papilledema) in a patient with idiopathic intracranial hypertension (IIH). A) Grade 4 papilledema in the patient’s right eye, marked by circumferential disc elevation, and obscuration of vessels both on the disc and leaving the disc. Disc hemorrhages are also present. B) Grade 4 papilledema in the left eye with disc hemorrhages.Text:
Disc edema is an ophthalmoscopic finding defined by unilateral or bilateral swelling of the optic disc. There are several synonyms used to describe this finding including papillitis, papilledema, swollen or choked discs, and the most commonly used term – optic disc edema (ODE). Optic disc edema presents with a buldging of the optic disc seen on fundus exam and may lead to loss of vision (Figure 1).
Presentation: Patients with ODE are often asymptomatic but can present with a range of symptoms based on the underlying cause. For example, a patient who has disc edema due to increased intracranial pressure (ICP) may present with positional headache, visual obscurations, or pulsatile tinnitus. If the cause in infectious, systemic symptoms may be present. As for visual symptoms, patients can present with decreased visual acuity, field defects, and a relative afferent pupillary defect when the disc swelling is asymmetric or unilateral.
Differential Diagnosis: It is useful to separate differential diagnoses associated with ODE into unilateral disc edema or bilateral disc edema.
Table 1: Causes of unilateral optic disc edema
| Cause | Symptoms | Fundus findings |
| Anterior Ischemic optic neuropathy (AION) | Arteritic AION: scalp tenderness, jaw claudication, fever, joint pains – associated with Giant cell arteritis.
Non-arteritic AION: history of vascular risk factors (Diabetes, Hypertension, Hyperlipidemia) |
Arteritis AION: Unilateral optic disc edema with a white, chalky appearance.
Non-arteritic AION: Unilateral optic disc edema, cup-less “disc at risk” in the fellow eye |
| Neuroretinitis | Viral URI symptoms, fever, lymphadenopathy, rash | Optic disc edema with a macular star |
| Papillitis/Optic Neuritis | Orbital pain with visual changes (blurring, field defect, or decreased color vision) and an afferent pupillary defect | Usually only optic disc edema |
| Papillophlebitis | Young, healthy patient with blurred vision, with or without a field defect | Optic disc edema, venous dilation, and disc hemorrhages |
| Retinal Vein Occlusion | History of vascular risk factors (Diabetes, Hypertension, Hyperlipidemia), sudden painless vision loss, afferent pupillary defect | Optic disc edema with dilated and tortuous vessels, extensive retinal hemorrhages, cotton wool spots |
Table 2: Causes of bilateral optic disc edema.
| Cause | Symptoms | Fundus Findings |
| Increased intracranial pressure (Papilledema) | Headache, pulsatile tinnitus, visual obscurations, nausea and vomiting | Bilateral optic disc edema |
| Diabetic Papillopathy | History of diabetes, visual changes (blurring or field defects) | Bilateral optic disc edema, microaneurysms, cotton wool spots, hard exudates, retinal hemorrhages, neovascularization |
| Hypertensive Papillopathy | History of hypertension, visual changes (blurring or field defects), headache | Bilateral optic disc edema, cotton wool spots, hard exudates, retinal hemorrhages, arteriosclerosis |
| Pseudopapilledema (Optic Disc Drusen) | Generally asymptomatic | Round, white/yellow bodies on and buried in the optic nerve head |
Diagnosis: A fundoscopic exam is crucial for diagnosing disc edema. In general, a fundoscopic or slit lamp exam will reveal enlarged retinal venules, blurred disc margins, elevation of the optic disc, obscuration of blood vessels traveling through the optic disc, and in severe cases, hemorrhage overlying the optic disc. Other fundus findings are specific to the underlying etiology. Optic disc edema is graded based on severity using the modified Frisén scale, shown in Figure 2. These findings together with patient symptoms and history are key to arriving at the proper diagnosis. These differentiating factors are described in Tables 1 and 2, above.
Unexplained optic disc edema necessitates further imaging studies. An MRI and MRV of the brain will evaluate for the presence of increased intracranial pressure including structural lesions and venous outflow obstruction, which can both lead to papilledema. A lumbar puncture may also be needed to evaluate for infection and elevated ICP. The presence of elevated ICP in the absence of a cause found on imaging may lead to the diagnosis of idiopathic intracranial hypertension, also known as pseudotumor cerebri.

Figure 2. Modified Frisén scale for grading of optic disc edema and papilledema. Key features of each grade are marked with an asterisk (*).
Management/Treatment: The management of disc edema is largely dependent on the causative agent. For example, antihypertensive medications can be administered for disc edema due to hypertension. Disc edema due to inflammatory causes can be treated with corticosteroids or immunosuppressive drugs. Infectious causes should be treated with an appropriate antibiotics. Treating the underlying condition will usually reduce disc edema and prevent progression to optic atrophy and permanent optic nerve damage.
Complications: The main complication with disc edema is permanent blindness secondary to optic atrophy. Disc edema typically only progresses to optic atrophy and irreversible blindness if left untreated for an extended period of time, leading to death of axons in the optic nerve. The speed of this progression is also dependent on the degree of disc swelling.
Faculty Approval: Griffin Jardine, MD
Identifier: Moran_CORE_26589
References:
- Chan JW. Optic Nerve Disorders: Diagnosis and Management. 1. Aufl. ed. New York: Springer; 2007;2008
- Frisén L. Swelling of the optic nerve head: a staging scheme. Journal of Neurology Neurosurgery Psychiatry 1982; 45:13.
- Van Stavern GP. Optic Disc Edema. Seminars in Neurology. 2007;27:233-243.
- Khurana KA, Aruja K, Khurana B. Comprehensive ophthalmology 6th edition. New Delhi: Jaypee, The Health Sciences Publisher.
- Lee AG, Beaver HA. Acute Bilateral Optic Disk Edema with a Macular Star Figure in a 12-Year-Old Girl. Survey of Ophthalmology. 2002;47:42-49.
- Newton PN, Thai LH, Tip NQ, et al. A Randomized, Double-Blind, Placebo-Controlled Trial of Acetazolamide for the Treatment of Elevated Intracranial Pressure in Cryptococcal Meningitis. Clinical Infectious Diseases. 2002;35:769-772.
- Sadun AA, Currie JN, Lessell S. Transient visual obscurations with elevated optic discs. Ann Neurol 1984; 16:489.
- Tso MO, Hayreh SS. Optic disc edema in raised intracranial pressure. IV. Axoplasmic transport in experimental papilledema. Arch Ophthalmology 1977; 95:1458.
- Wall M. Idiopathic Intracranial Hypertension. Neurologic Clinics. 2010;28:593-617.
Examination of the Red Reflex in Pediatric and Adult Patients
Home / Basic Ophthalmology Review / Direct Ophthalmoscope
Title: Examination of the Red Reflex in Pediatric and Adult Patients
Author (s): Cole Swiston, MSIV, University of Wisconsin School of Medicine and Public Health
Photographer: Ethan Peterson (Videographer), James Gilman CRA/FOPS (Photographer)
Date: 09/17/2018
Learning Objectives:
- Understand the basic physics and physiology which result in the red reflex
- Learn the purpose of red reflex testing in pediatric and adult patients
- Learn how to perform red reflex testing with the direct ophthalmoscope (see our video on the use of the direct ophthalmoscope for more details on its general use)
- Become familiar with basic etiologies of an abnormal red reflex in pediatric and adult patients
Description:
The red reflex is a reflective phenomenon seen when light passes through the pupil and is reflected back off the retina to a viewing aperture, creating a reddish orange glow. You may notice this commonly in pictures with flash. Red reflex testing is a valuable tool for detection of abnormalities in the normally transparent visual axis or in the retina. Loss of transparency in any of these structures can alter the red reflex, including from front to back; the tear film, cornea, aqueous humor, lens, vitreous gel, and retina. In pediatric patients, abnormalities in the red reflex can be the first clue to sight threatening conditions that cause amblyopia, or life-threatening pathologies such as retinoblastoma. Similarly, the red reflex can assist in the diagnosis of conditions causing visual loss in adults.
When examining the red reflex, look first for its presence or absence, the color of the reflex, brightness, and importantly, symmetry between eyes.
How to perform red reflex testing:
- Make sure the lights in the room are turned off, making the red reflex easier to see.
- Align the height of your eyes with the patient’s eyes. If the patient is a child, have them sit on their parent’s lap.
- Set your direct ophthalmoscope diopter power to 0, or to match your refractive error.
- Switch on the ophthalmoscope, hold it close to your eyes and 12-18 inches away from the patient’s eyes, and shine the light towards the patient’s eyes.
- Encourage the patient to look at your light. Toys and hand motions may be helpful.
- Direct your light at each eye individually to evaluate the red reflex of each eye.
- Direct your light over both eyes to evaluate for symmetry of the reflex.
The American Academy of Pediatrics recommends red reflex testing in all patients during the neonatal period and during all subsequent well child and routine health appointments. Any abnormalities discovered, especially leukocoria, require urgent referral to an ophthalmologist.
Leukocoria is a term for whitening of the red reflex. The most common conditions causing this whitening are retinoblastoma (a serious tumor in the back of the eye), cataracts, persistent fetal vasculature and Coat’s disease. Coat’s disease is characterized by abnormal blood vessel development in the retina and can threaten vision if left untreated. Another important aspect of red reflex testing is evaluating for symmetry between eyes. Asymmetry would be considered an abnormal result and is generally evaluated with the Bruckner test, where both eyes are visualized simultaneously with the direct ophthalmoscope. In strabismus, or misalignment of the two eyes, the deviated eye will generally have a lighter and brighter red reflex. If the refractive error is different between the two eyes (termed anisometropia), one reflection also may be brighter than the other. It is especially important to evaluate for these conditions, as they both may lead to amblyopia, which is abnormal development of the normal visual pathways. Similar to a pediatric patient, dimming, dulling, or asymmetry in an adult patient often indicates opacity of structures in the visual axis. The most common cause of this dulling in an adult is a cataract, but an abnormal red reflex may also clue you in to other pathologies in the cornea (abrasion, infection, or scar), vitreous (hemorrhage or inflammation), or retina (retinal detachment).
Format: Video
References:
- Ophthalmology S on. Red Reflex Examination in Infants. Pediatrics. 2002;109(5):980-981. doi:10.1542/peds.109.5.980
- How to test for the red reflex in a child. Community Eye Health. 2014;27(86):36.
- Shafiq A. Seeing red in young children: the importance of the red reflex. Br J Gen Pr. 2015;65(633):209-210. doi:10.3399/bjgp15X684625
- Light Reflex Tests. https://www.aao.org/bcscsnippetdetail.aspx?id=703d090d-b6a0-45d5-a3da-e456c030caec. Accessed September 6, 2018.
Faculty Approval by: Griffin Jardine, MD
Copyright statement: Cole Swiston, ©2018. For further information regarding the rights to this collection, please visit: http://morancore.utah.edu/terms-of-use/
Identifier: Moran_CORE_25760
Anterior Chamber Depth Penlight Estimation
Home / Basic Ophthalmology Review / Penlight Examination
Home / Basic Ophthalmology Review / Anterior Chamber
Title: Anterior Chamber Depth Estimation with a Penlight Examination of the Red Reflex in Pediatric and Adult Patients
Author: Alex Compton, MSIV, Texas Tech University Health Sciences Center
Date: 10/05/2018
Photographer: Ethan Peterson (Videographer), James Gilman CRA/FOPS (Photographer)
Keywords/Main Subjects: Anterior chamber; Penlight examination
Secondary CORE Category: Basic Ophthalmology Review / Anterior Chamber
Diagnosis: N/A
Brief Description: This video explains the key anatomical structures in the anterior eye, describes the use of the penlight in examination of the eye and demonstrates how the penlight can be used to estimate anterior chamber depth.
Format: mp4
Series: Basic Ophthalmology Review, Medical Student Outline
Identifier: Moran_CORE_25690
Copyright statement: Copyright 2018. Please see terms of use page for more information.
Lid Lag and Stare
Home / Basic Ophthalmology Review / Lids/Lashes
Title: Lid Lag and Stare
Author (s): Zachary Mortensen, MS4, MBA
Photographer: James Gilman
Date: August 24, 2018
Keywords/Main Subjects: lid lag, stare, Von Graefe’s, graves’ ophthalmopathy, thyroid eye disease, graves’ orbitopathy, lagophthalmos
Diagnosis: Thyroid eye disease (hyperthyroidism, Graves’ orbitopathy, graves’ ophthalmopathy)
Introduction
Lid lag, Von Graefe’s sign, stare, and lagophthalmos can be useful eyelid findings when evaluating a patient with thyroid eye disease. While they characteristically occur in patients with Graves’ disease, it is important to note that these signs are not pathognomonic for thyroid eye disease.1 Lid lag can be less commonly caused by congenital blepharoptosis from a fibrotic levator muscle, and lagophthalmos can occur from a lesion to the facial nerve or iatrogenically from an overaggressive upper blepharoplasty.2,3
Graves’ orbitopathy or thyroid eye disease is an autoimmune disorder that occurs in about 1/4th of patients with a hyperactive thyroid in Graves’ disease.4 However, thyroid eye disease can sometimes occur in patients with hypothyroidism (e.g., Hashimoto’s).5 In Graves’ disease, the thyroid-stimulating hormone receptor antibodies activate fibroblasts in the tissues behind and around the eye or globe. This results in inflammation, swelling, and volume expansion of the retroorbital tissues. This tissue presses on the back of the eye causing it to be pushed out. This bulging of the eye anteriorly is known as “proptosis” or “exophthalmos”. Lid lag and stare, however, are believed to be caused by excess thyroid hormone and not necessarily from the proptosis.6 The elevated thyroid hormone levels are believed to increase the contraction of the eyelid muscles, which is likely why treatment of the hormone levels can relieve the symptoms of lid lag and stare.6
The active phase is marked by eye redness, pain, and swelling. These symptoms can increase and decreases in intensity during this phase. Smoking cessation is important in management as the phase typically lasts 1 year for non-smokers and 2-3 years for smokers.5
Lid Lag
Lid lag is a static condition in which the upper eyelid is higher than normal while the eye is in downgaze.7 Lid lag can be measured by comparing the upper eyelid position in downgaze to its position in primary gaze relative to a fixed point like the pupil.1 Lid lag happens when there is increased contraction of the levator palpebrae muscles of the eyelids.6 Lid lag subsides when the hyperthyroidism is treated.6
A term often confused with lid lag is von Graefe’s sign. Von Graefe’s sign is dynamic rather than static.7 It is observed when the eye actively moves inferiorly from primary gaze and the upper eyelid follows at a slower-than-normal rate. The superior part of the iris (superior limbus) is often exposed during this slowed movement.1 Once the downgaze is fixed, and if the eyelid remains elevated, it may then be called “lid lag”.

Figure 1: A 57-year-old man with Graves’ thyroid eye disease. He has scleral injection and asymmetry in proptosis and lid positions. His lid lag is most apparent on downgaze as the lids do not entirely cover the superior limbus, iris, or pupil. Note the hyper-retracted upper eyelids.
Stare
Stare is the term used to describe the appearance of a patient with excessive eyelid retraction.6 The increased tightness of the levator palpebrae that causes lid lag can also give the patient this “staring” appearance. It is important not to confuse this with proptosis (bulging of the eye out of the socket) as they are two distinct conditions and can occur one without the other.6 Stare, like lid lag, subsides when the hyperthyroidism is treated.6

Figure 2: A 57-year-old man with Graves’ thyroid eye disease in relaxed primary gaze demonstrating stare. While the left eye appears more proptotic (bulging), both eyes have increased lid tightness. Normal eyelids would appear more relaxed.

Figure 3: A 68-year-old woman with bilateral Graves’ orbitopathy, status post thyroidectomy, taking levothyroxine, with residual mild diplopia and mild proptosis. Note that her upper eyelids are so tightly retracted that they are hardly visible, giving her the classic stare.
Lagophthalmos
Lagophthalmos is the inability to completely close the eyelids.1 Excessive upper lid retraction in thyroid eye disease can result in lagophthalmos and corneal exposure even while the patient attempts to close their eyes.

Figure 4: A 57-year-old man with Graves’ thyroid eye disease has upper lid retraction with mild lagophthalmos of the left side and some corneal exposure
References:
- Gaddipati, R. V., & Meyer, D. R. (2008). Eyelid Retraction, Lid Lag, Lagophthalmos, and von Graefe’s Sign: Quantifying the Eyelid Features of Graves’ Ophthalmopathy. Ophthalmology, 115(6), 1083-1088.
- Salman, M. S., & Clark, I. H. (2017). Eyelid Retraction in Isolated Unilateral Congenital Blepharoptosis. Frontiers in neurology, 8, 190.
- Shorr, N., Goldberg, R. A., McCann, J. D., Hoenig, J. A., & Li, T. G. (2003). Upper eyelid skin grafting: an effective treatment for lagophthalmos following blepharoplasty. Plastic and reconstructive surgery, 112(5), 1444-1448.
- Tanda, M. L., Piantanida, E., Liparulo, L., Veronesi, G., Lai, A., Sassi, L., … & Bartalena, L. (2013). Prevalence and natural history of Graves’ orbitopathy in a large series of patients with newly diagnosed Graves’ hyperthyroidism seen at a single center. The Journal of Clinical Endocrinology & Metabolism, 98(4), 1443-1449.
- Liaboe CA, Clark TJ, Shriver EM, Carter KD. Thyroid Eye Disease: An Introductory Tutorial and Overview of Disease. org. posted November 18, 2016; Retrieved August 23, 2018, from: http://www.EyeRounds.org/tutorials/thyroid-eye-disease/
- Davies, T.F., Burch, H. B., Ross, D. S. (2018). Clinical features and diagnosis of Graves’ orbitopathy (ophthalmopathy). In J Mudler (Ed.), UpToDate. Retrieved August 23, 2018, from https://www.uptodate.com/contents/treatment-of-graves-orbitopathy-ophthalmopathy?topicRef=7825&source=see_link#H17628836
- Harvey, J. T., & Anderson, R. L. (1981). Lid lag and lagophthalmos: a clarification of terminology. Ophthalmic Surgery, Lasers and Imaging Retina, 12(5), 338-340.
Copyright Zachary Mortensen, ©2016. For further information regarding the rights to this collection, please visit: URL to copyright information page on Moran CORE
Disclosure (Financial or other): none
Identifier: Moran_CORE_25597
Eyelid Masses
Home / Basic Ophthalmology Review / Lids/Lashes
Title: Eyelid Masses
Author: Xavier Mortensen, MS4, University of Utah School of Medicine
LOCATION: Medical Student Education Outline > II. Anatomical Approach to Eye Disease > Lids/Lashes > 4. Masses
Eyelid Masses
Eyelid masses can be categorized into inflammatory, benign, or malignant masses. Below is a description of some of the more common masses found in each of these categories.
Inflammatory Masses
Chalazion
A chalazion is an inflammatory—but typically not infectious—mass of the eyelid that results from an obstruction of the Meibomian glands. It often presents with a dome-like elevation with surrounding erythema. The Meibomian glands are the oil-producing sebaceous glands on the posterior margin of the upper and lower eyelids. It can be associated with intense inflammation and therefore can be painful. If there is a superimposed bacterial infection, it may be purulent. It is commonly associated with rosacea and chronic blepharitis.
Treatment: Warm compress with gentle massage in addition to eyelid hygiene. Minocycline or doxycycline may be used for multiple and recurrent cases. It may take weeks to months to resolve fully.
Stye (External Hordeolum)
A stye is an acute infection of the sebaceous glands (glands of Zeis or Moll) of the anterior margin of the eyelid (often Staphylococcus aureus). It often appears to center around an eyelash follicle. It can be painful, hot, and swollen.
Treatment: Spontaneous resolution often occurs; however warm compresses and topical antibiotic ointment may be used if needed.
Benign Eyelid Lesions/Tumors
Squamous Papilloma
This is the most common benign eyelid tumor growth. The lesion is skin colored and can either be sessile or pedunculated. Pathology reveals epithelial hyperkeratosis and acanthosis around a central vascular core. It grows slowly and often forms groups of tumors in children, while in the elderly it more commonly is isolated as individual tumors or widely spaced tumors. The etiology isn’t completely understood, but increased age is a risk factor and may be associated with viruses in children.
Treatment: Complete excision
Verruca Vulgaris
This lesion is caused by infection by the human papillomavirus (often 6, 11, or 16). It presents as a pedunculated or sessile hyperemic mass on the eyelid with minimal surrounding inflammation. This lesion has potential for malignancy.
Treatment: Observe if small. Larger lesions can be excised, scraped, cauterized, or cryotherapy.
Moll’s Gland Cyst
This is caused by abnormal proliferation of moll’s gland. It appears smooth, translucent, and is slow growing and painless. It is more common in adults than children.
Treatment: marsupialization or complete excision
Malignant Eyelid Tumors
Basal Cell Carcinoma
This is the most common eyelid malignancy. It is most often found on lower eyelid and medial canthus region. Classic description: pearly border, telangiectasia, may ulcerate. Prolonged sun exposure, history of cigarette smoking, fair skin, are risk factors. It often presents in the middle-aged or elderly.
Treatment: Complete excision, Mohs surgery. Topical imiquimod. Protect against further sun damage.
Squamous Cell Carcinoma
This is much less common compared to basal cell carcinoma. Male gender, sun exposure, fair skin, immunosuppression, and radiation are risk factors. These present as a scaly, ulcerated, erythematous plaque that is most often found on the lower eyelid and lateral canthus region. It can be confused with basal cell carcinoma, but it usually does not have superficial vascularization, grows more rapidly, and hyperkeratosis is more frequent.
Treatment: Incisional or excisional biopsy. Adjunctive radiation, cryotherapy, or chemotherapy can be used as well. Protect against further sun damage.
Sebaceous Carcinoma
This is a highly malignant neoplasm that arises in the Meibomian or Zeiss glands. More common in older people (7th, 8th decade), females (2X as likely as males) and is more commonly found on the upper eyelid. It is often referred to as the “great masquerader” as it can present similarly to chronic blepharitis, recurrent chalazion, or basal or squamous cell carcinoma. These patients present with madarosis (eyelid loss), poliosis (skin or hair color de-pigmentation), and thick lid margin inflammation. Tumors can be yellow and hard. Lymphadenopathy is common.
Treatment: Wide surgical excision. Map biopsies of conjunctiva. Orbital exenteration is required in severe cases.
Malignant Melanoma
These often present as a dark, variable pigmented nodule or plaque with irregular, notched borders. Risk factors include sunlight exposure, genetic predisposition, and environmental mutagens. These are the most lethal primary skin tumors, but are rare (<1% of eyelid malignancies).
Treatment: Incisional or excisional biopsy or complete excision.
References:
- Bagheri, Nika, et al. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 7th Edition. Philidelphia: Wolters Klewer, 2017.
- Carreiro de Freitas, Ana Vega, Cat Nguyen Burkat and Simantha Khadka. Squamous Carcinoma of the Eyelid. 6 May 2016. 28 June 2018. <http://eyewiki.org/Squamous_Carcinoma_of_the_Eyelid>.
- Kaiser, Peter K, Neil J Friedman and Roberto Pineda. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 4th Edition. Elsevier Inc., 2014.
- Skuta, Gregory L, Louis B Cantor and Jayne S Weiss. “Basic and Clinical Science Course.” Section 7: Orbit, Eyelids, and Lacrimal System. 2010-2011. American Academy of Ophthalmology, 2010. 164-166, 169-170, 181-190.
Photography Credit:
Chalazion, Squamous Papilloma: Douglas Marx, MD
Stye, Basal Cell Carcinoma, Sebaceous Carcinoma: Alison Crum, MD
Identifier: Moran_CORE_25570