What is an acrochordon or skin tag and how do you treat it?
Home / Orbit, Eyelids, and Lacrimal System
Contributors: BCK Patel MD, FRCS, Jay Patel BSC, Raman Malhotra FRCS
Photographer: BCK Patel MD, FRCS
Introduction

Fig 1: Acrochordon: lesions of many kinds are common on the eyelids, cheek and in the periorbital area in general. 1. Acrochordon caused by actinic keratosis 2. Vascular nevus 3. Dermal flat papilloma 4. Pigmented nevus 5. Keratotic acrochordon
Acrochordons are benign pedunculated lesions which may arise anywhere on the body. The colloquial term for it is “skin tag”. The proper medical term is “fibroepithelial polyp”, often abbreviated to “FEP”. They commonly occur on the neck, the axilla and the groin regions. Acrochordons are associated with obesity. On the face, they are most often noticed by patients when they occur on the eyelids.

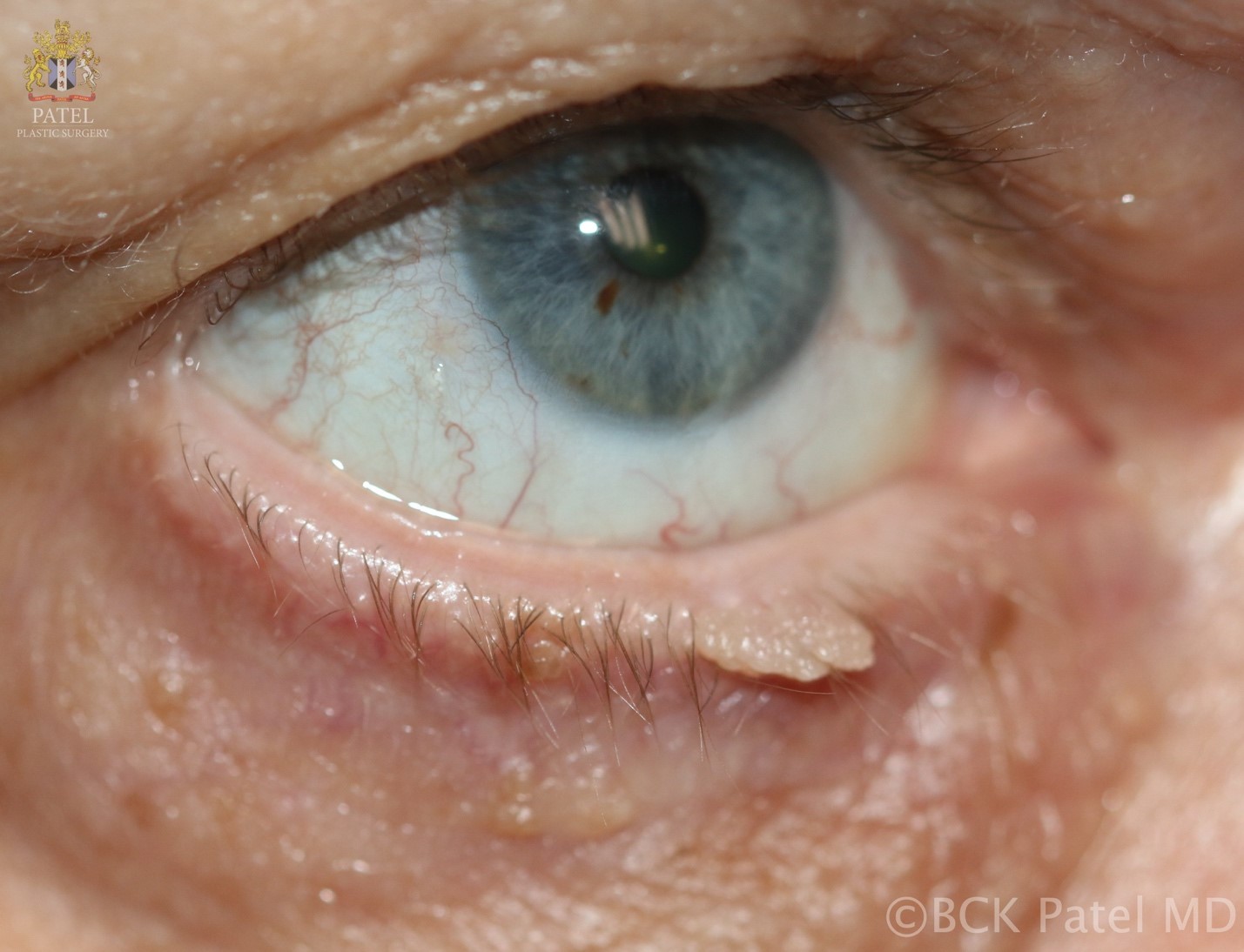
Fig 2: Acrochordon or large “skin tag”: histopathologically, this acrochordon could be a squamous papilloma or a viral papilloma

Fig 3: Depiction of an acrochordon: a lesion with a head and a thinner stalk, often described as “pendulous”
It should be noted that the term “acrochordon” is a descriptive term and does not imply any particular histopathology. Some terms, like “basal cell carcinoma”, are specific terms which imply a particular type of histopathology. Therefore, the term acrochordon may be applied to many different histopathological conditions which manifest themselves with the macroscopic appearance of “a pedunculated lesion”.
Etymology
Acrochordon is derived from the Greek “acro-“, meaning top or summit, and “chorde” meaning cord or string. Since acrochordons are pedunculated with a narrow stem and an enlarged head, the descriptive derivation of “acrochordon” makes perfect sense. However, the classical Greek spelling is “akrochordṓn ”, while the Latin is “acrochordō.’
The classical Latin “acrochordon” was used by Aulus Coenelius Celsus (c. 25 BC – c. 50 AD) and the ancient Greek ἀκροχορδών derived from ἄκρο- and χορδή by Hippocrates of Kos (c. 460 BC – c. 370 BC).

Fig 6: The textbook “Chirugia parva Lafranci” by John Halle (1529 – 1569) – the name “Halle” was often spelled “Hall” in his manuscripts. He was the first used the term “acrochordon”
The earliest use of the term “acrochordon” in the English language was by the poet and physician, John Halle (1529 – 1569), a man ahead of his times in his thinking, who practiced in Maidstone, Kent. His medical textbook Chirurgia parva Lanfranci published in London in1565 presented for the first time in detail, medical ethics, discussed the importance of obtaining second opinions and stressed the “primacy of experience over book learning” when studying Medicine. He also exposed charlatans and decried fraudulent medicine. At the time, medical textbooks often had to be referred to the Church for approval before publication. Halle would have been familiar with the fate of Michael Servetus, the Spanish physician, theologian and humanist who published his theory on the circulation of blood between the heart and the lungs, leading to his condemnation to death for heresy (for this and other perceived religious transgressions – “execrable blasphemies” as termed by John Calvin, his main prosecutor). Servetus “was burnt alive – atop a pyre of his own books – at the Plateau of Champel at the edge of Geneva” in 1553. Therefore, many physicians of the time, including Halle, published their medical textbooks disguised as new translations of earlier writings, to avoid censure.

Fig 7: A typical page from John Halle’s textbook with dense text in “Olde English”. These textbooks were usually published in Latin and Olde English. This textbook, like many of this time had no illustrations. Because of the rarity of medical textbooks, these would be read and studied cover-to-cover by medical students and physicians.
The use of the term “acrochordon” subsequently disappeared until around 1800, after which it became more ubiquitous, only to fall into disuse in the 20th century, with a subsequent resurrection in the 21st Century!
Acrochordon is frequently misspelled “achrochordon” or “Achrocordon” in the English medical literature. In Spanish, the correct spelling is “acrocordón”, “acrocordone” in Italian, and “acrocórdon” in Portuguese.
Synonyms
- Skin tag
- Papilloma
- Fibroma pendulum
- Fibroepithelial polyp
- Molluscum fibrosum pendulum
- Filoform benign mole
Etiology
It was thought that areas with poor elastic tissue results in atrophy and also sessile lesions. As these sessile lesions increase with age, it was thought that the loss of elastic tissue with age may have a bearing on their increased occurrence. However, histological studies have failed to confirm this.

Fig 9: Typical acrochordon (skin tag) on the left upper eyelid with two smaller ones supero-lateral to the larger one.
Hormonal imbalances have also been implicated, such as elevated estrogen and progesterone levels in pregnancy and high levels of growth hormone in acromegaly. Also, epidermal growth factor (EGF) and alpha tissue growth factor (TGF) have been associated with an increased incidence of acrochordons.
Viral infections have been implicated by the finding of human papillomavirus (HPV) in a high percentage of skin tag biopsies. Skin infections are thought to promote the growth of these lesions as well. Local trauma may be responsible for increased occurrence of arcochordons by the release of mast cell mediators.
A rare autosomal dominant condition called Birt-Hogg-Dube (BHD) syndrome is characterized by fibrofolliculomas, trichodiscomas and acrochordons. Renal and colon carcinomas can occur.
Contrary to initial reports, there is no association of acrochordons and colonic polyps.
Skin tags have been associated with type 2 diabetes mellitus with an incidence of 40.6% of type 2 diabetes mellitus or impaired glucose tolerance in a study of patients with acrochordons.

Fig 10: Close-up of a right upper eyelid acrochordon showing the typical narrow stem and bulbous head
Epidemiology
Acrochordons increase with age and are known to occur in 46% of the general population with an equal occurrence in males and females. The incidence of the lesions increases with age with more than 60% of people having these lesions by the 8th decade. They occur more commonly in diabetics and in obese patients. Patients will frequently have a family history of skin tags. Other factors associated with increased incidence of skin tags includes dyslipidemia, insulin resistance, elevated C-reactive protein and hypertension.

Fig 11: Multiple acrochordons and a hydrocystoma on the left lateral canthal region and fibrous nodules in the left temple. This cystic lesion is not a cyst of Moll because the lesion is away from the eyelid margin where the glands of Moll reside as do the cysts of Moll
Differential Diagnosis
Squamous papillomas, viral warts, benign melanocytic nevus, and neurofibromas may all present as soft pedunculated lesions. Pedunculated nevi and pedunculated seborrheic keratoses can resemble acrochordons on the face, especially the variant called dermatosis papulosis. These are most commonly seen in Fitzpatrick type VI skin. A variant of basal cell carcinoma, fibroepithelioma of Pinkus is a basal cell carcinoma which can look like a pink acrochordon and occurs on the lower back.

Fig 12: Fibroepithelioma of Pinkus and basal cell carcinoma (first described by Hermann Pinkus in 1953. Although this is relatively flat, rasied areas can imitate an acrochordon (Image with kind permission from the South Tees Hospitals NHS Foundation Trust, England)
Hermann Pinkus (born in 1905 in Berlin) and his father Prof. Felix Pinkus were both trail blazers in the field of dermatopathology. Hermann Pinkus also described the eccrine poroma and coined the term “acrosyringium” which essentially described the epidermal sweat duct unit.
Nodular melanomas have been known to present in the form of an acrochordon. Squamous cell carcinoma is rare but may be seen at the base of an acrochordon. Studying 1335 clinically diagnosed acrochordons, four were found to be basal cell carcinomas and one was a squamous cell carcinoma.
So the list of histopathological conditions that can look like an acrochordon on the body is impressive:
- Squamous papilloma
- Benign melanocytic nevus
- Neurofibroma
- Adenoma sebaceum
- Melanocytic nevi
- Solar lentigines
- Syringomas
- Trichoepithelioma
- Verrucae
- Dermatosis papulose nigra
- Pseudosarcomatous polyp.
- Melanoma metastases
- Dermatofibroma
- Keratoacanthoma
- Pedunculated seborrheic keratoses

Fig 15: An acrochordon growing on a base of seborrheic keratosis, also called a pedunculated seborrheic keratosis
- Skin-tag like basal cell carcinomas can be seen in the basal cell nevus syndrome.
- Squamous cell carcinoma should be excluded in the presence of large acrochordons, especially with superficial bleeding.
- Nevus lipomatosis cutaneous superficialis is a benign hamartomatous disorder.
- Mycosis fungoides has been shown to involve an acrochordon with known mycosis fungoides.
- Genital warts will have the clinical appearance of acrochordons.
- Melanocytic nevi can have extensions that can resemble acrochordons.
- Non-genital warts
- Pinkus tumor
Pathophysiology
Previous theories have suggested that a localized paucity of elastic tissue may result in sessile or atrophic lesions. It is also thought that pendulous variations may be caused by losses of large confluent areas of elastin; however, a study of elastic tissue in fibroepithelial polyps (FEPs) showed no significant abnormalities.
A cross-sectional study of adult patients at a university teaching hospital, including 98 patients and 103 controls, found that the presence of multiple skin tags was strongly associated with insulin resistance, irrespective of other risk factors. [1]
In another survey, 113 patients with skin tags and 31 healthy subjects were evaluated. This work linked obesity, dyslipidemia, hypertension, insulin resistance, and elevated high-sensitive C-reactive protein with skin tags, suggesting they may serve as a marker of increased risk of atherosclerosis and cardiovascular disease.[2, 3]
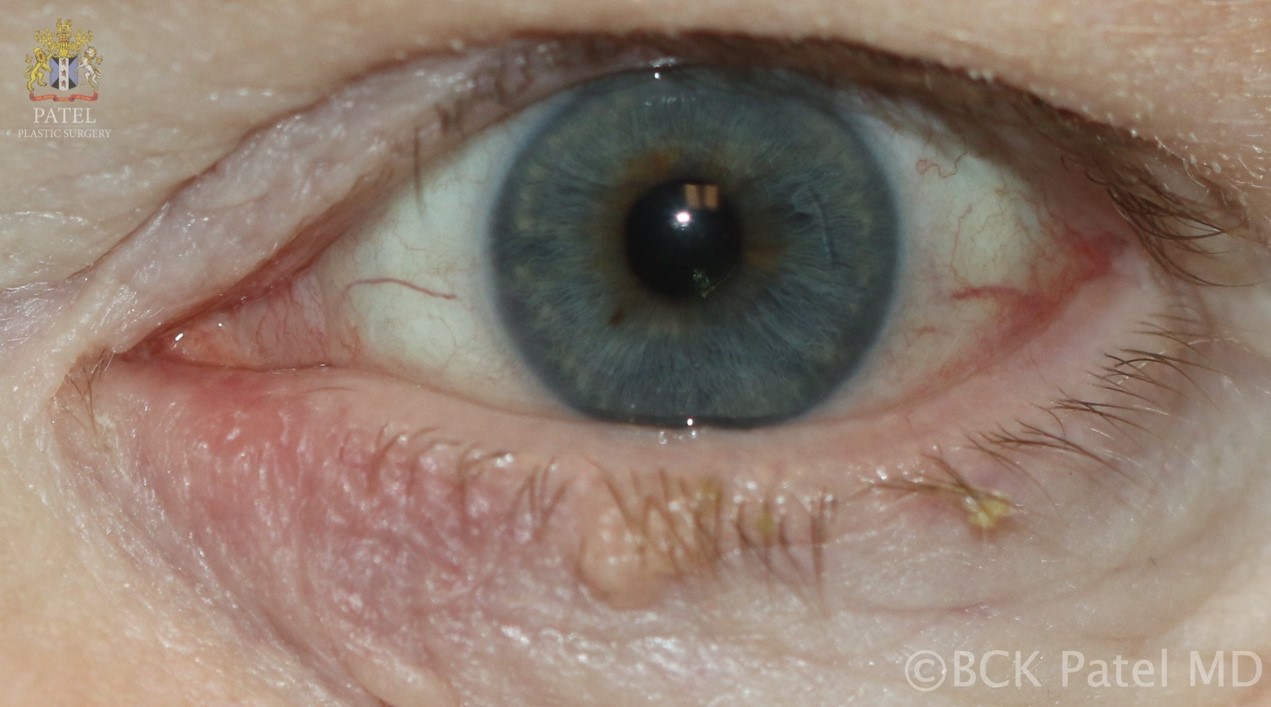
Fig 16: A left lower eyelid central seborrheic keratosis evolving into a prominence which will go on to develop into an acrochordon. Note the small lateral lower eyelid acrochordon
Histopathology
Histopathology will reveal acanthosis with frond-like epithelium. The dermis will show loosely arranged collagen fibers with lymphatic vessels and capillaries but none of these findings are diagnostic. As the diagnosis of acrochordon affecting eyelids and the periorbital region is a clinical one and as these are benign lesions, histopathology is rarely obtained.
Bottom: Low magnification of the lesion showingacanthotic epithelium with crypts and cysts filled with keratin (With thanks to Prof. Nick Mamalis MD)

Fig 18: Acrochordon histopathology higher magnification. Top: Fibrovascular cores and keratin-filled crypts. Bottom: Fibrovascular cores within the lesion that extend from the dermis to the epidermis (With thanks to Prof. Nick Mamalis MD)
Clinical Findings
Acrochordons may occur anywhere on the body, with the neck, axillae, the groins, the trunks and the face being the most common. They commonly affect the eyelids and periorbital regions, increasing with age. They present as pedunculated, soft lesions which may be skin-colored, pale or hyperpigmented. They are usually 2 – 5 mm in diameter, although occasionally, “giant acrochordons” may be found measuring more than 1 cm in diameter and in some parts of the body, they may grow to as large as 18 cm.
Clusters of skin tags can occur, usually in the intertriginous zones of the axillae, under breasts, and the groin region. The commonest presentation is a cosmetic complaint. However, lesions can break down when on the back or the groins, causing irritation and discomfort. Local inflammation may be seen with trauma to the lesions in pressure-bearing zones.
Acrochordons have been divided into:
- Small lesions 1 – 2 mm in width and height. These are found on the face, neck and the axillae
- Single or multiple lesions 2 mm to 5 mm in length which can occur anywhere on the body
- Large pedunculated lesions which may be as large as 2 – 5 cm and occur on the lower trunk.
Acrochordons have been found in the vulval region where they can grow to a large size, the penis, anus and even in the urethra. Skin tags have also manifest themselves as “a hill upon a hill” and have been found on prolapsed hemorrhoids.

Fig 20: Multiple different lesions from flat keratoses to pigmented nevi to acrochordons on the left side of the neck. These are more common as we age, especially in the intertriginous areas
Acrochordons will often coexist with the hyperpigmented, velvety thickening of the skin that may be seen in the intertriginous zones: neck, axillae, groins, breasts. This is caused by stimulation of epidermal keratinocytes and dermal fibroblast proliferation. Acanthosis nigricans may be associated with insulin resistance, especially in young patients. In older patients, acanthosis nigricans can be associated with an internal malignancy, usually gastrointestinal. Acanthosis nigricans is often seen with obesity, hyperinsulinemia and craniosynostosis. Treatment of any metabolic abnormality and weight loss will result in regression of acanthosis nigricans.

Fig 21. Acanthosis nigricans of the armpit. Note the acrochordons (circled). Courtesy of the Primary Care Dermatology Society (https://www.pcds.org.uk/clinical-guidance/acanthosis-nigricans#introgallery-1)
Investigations
Acrochordons do not require any specific investigations. In the presence of pigmentation, it is reasonable to obtain histopathology to exclude melanoma. Similarly, in lesions with obvious vessels, it is reasonable to exclude basal cell carcinoma. When multiple acrochordons are removed, it is unwise to send them all together for histopathology. If there is any suspicion, the lesions should be sent separately, together with a note to the pathologist explaining what the suspicion is and the exact location of the lesion.
Natural History
Skin lesions of all kinds increase as we age. Indeed, elevated skin lesions like actinic keratoses, seborrheic keratoses, acrochordons, and others are almost ubiquitous in our seventh and eight decades. (REF Iranian study). Untreated, acrochordons grow slowly. Over time, the pendulous nature of the lesions leads to superficial ulceration with secondary irritation and pain. Some of these lesions will fall off because of ischemia created at the narrow stalk.

Fig 22: A relatively flat squamous papilloma. These can, over time, develop a stalk and become acrochordons
Treatment / Management
Most acrochordons do not cause any symptoms. Patients may present with lesions that are irritated or for removal of the lesions for cosmetic concerns. Lesions may be irritated by clothing, seatbelts, jewelry or simply pressure when they occur on the back, causing discomfort.
Various skin tag removal bands, patches and creams are sold for “at home” use. They rely on cutting off the blood supply to the head of the acrochordon. Creams may contain salicylic acid, tea tree oil and other irritants which may cause contact dermatitis. Tea tree oil is soaked in a cotton ball which is fixed to the skin tag with a bandage. Local irritation causes ischemia to the acrochordon. This method should be avoided for lesions on the eyelid.
A similar treatment is the soaking of cotton balls with apple cider vinegar and fixation to the tag with a bandage for 10 minutes and repetition until the lesion falls off. Again, local irritation may occur and this method should not be used around the eyelids.
When using any such chemicals, the surrounding skin can be protected with petroleum jelly or coconut oil. Iodine has also been used to soak the lesion until it falls of but its efficacy is unknown.
In Asia and Africa, local treatments have included tying a thread or wire around the stalks of these pedunculated lesions and leaving the thread on until the lesions fall off. This is similar to the modern use of surgical thread to tie the base of the lesion, although this is less used now with more definitive modern techniques of excision.
Home remedies which have been recommended for the treatment of acrochordons but should be regarded with great trepidation include:
- burning the acrochordon with a match
- sharply pulling them off with tweezers
- biting them off (!)
- applying acid
- applying hemorrhoid cream (does not work)
- “sanding them down!”
Cryotherapy when applied to temperatures of −4°F to −58°F will lead to ischemia of the lesion. At home cryotherapy kits are available but there is a risk of causing freeze burns to the surrounding tissues if the application is not accurate. Liquid nitrogen in medical practices are applied with a spray or with cryo tweezers which are applied to the base of the skin tag.
An Example of how to use Cryo Tweezers:
https://youtu.be/HhsQxbazd68
An Example of how to use cryotherapy:
Not all skin tags are useless! Eley et al described the use of skin tags as a source of tissue to reconstruct a congenital nasal deformity. [5]
Simple cauterization with or without injection with local anesthetic may also be used but can be uncomfortable and there is a risk of local burns.
Electrodissection is the use of a high-voltage, low-amperage and high frequency current in a monoterminal fashion. It causes superficial dehydration of the tissue with most of the injury being epidermal. This allows the treatment of lesions like acrochordons with minimal surrounding tissue damage, thereby reducing the risk of scarring, compared to standard electrocautery. The treatment is performed with a low setting of the instrument. It should not be used when a patient has a cardiac pacemaker as malfunction may occur. Electrodissection can be performed with topical anesthetic or local injection anesthesia.
The simplest and most effective way of remove the acrochordons is with injection of local anesthetic to the base and sharp excision of the stalk at the root using Westcott scissors and with local application of cautery to control bleeding. Application of aluminium chlorite prior to removal of acrchordons may decrease bleeding. Topical ethyl chloride spray anesthesia may also be used instead of injection anesthesia.
Simple Excision:
Instruments:
-
- 2% lidocaine with epinephrine on a 30 or 32 gauge needle
- Monopolar cautery
- Westcott scissors and 0.5 mm forceps may be needed
- Gauze
Surgical Steps:
-
- Cleanse the area of the acrochordon with an alcohol wipe
- Apply the Gate theory (tapping, massage, rubbing of hands, arms, legs, etc) to reduce the perception of discomfort during the injection of local anesthetic
- Infiltrate the base of the lesion with local anesthetic
- Elevate the acrochordon with forceps
- Excise the lesion at the very root
- If there is oozing, simple local cautery may be applied
- Simple topical antibiotic ointment may be applied
- No dressing is required in most cases
After the Procedure:
-
- The treated area is usually kept open
- The area can be washed gently with regular soap and water
- An ointment (antibiotic ointment) or a moisturizer may be applied twice a day to keep the area moist as it heals
- A plaster may be applied if the healing area is obviously visible but keeping the healing area exposed to the air is best
- A scab may form which usually falls of in three to five days
- After the area is healed, simple moisturizer and a sunscreen with SPF of at least 30 us used to prevent hyperpigmentation of the area
Prognosis
As these are benign lesions, they do not need any monitoring. However, it is important to be aware of the other conditions that can present as an acrochordon. [6] After excision, recurrence in the same spot is uncommon although areas prone to suffer from repeated trauma have a tendency to grow acrochordons. [7] The patient should be warned that it is normal for newer lesions to appear over time but they are not transmissible. They do often present with family histories.
Summary
- Acrochordons are generally benign. However, they can be associated with other conditions.
- The commonest complaint is a cosmetic one although some can cause irritation.
- They increase with age.
- They are seen more often in patients who are overweight.
- Acrochordons are often seen in families.
- Acrochordons can indicate insulin resistance.
- Over time, new acrochordons do grow, especially in the intertriginous zones
References
- Bustan RS, Wasim D, Yderstræde KB, Bygum A. Specific skin signs as a cutaneous marker of diabetes mellitus and the prediabetic state – a systematic review. Dan Med J. 2017 Jan;64(1): A5316
- Barbato MT, Criado PR, Silva AK, Averbeck E, Guerine MB, Sá NB. Association of acanthosis nigricans and skin tags with insulin resistance. An Bras Dermatol 2012 Jan-Feb;87(1):97-104 PMID: 22481657.
- Crook M. Skin tags: a useful clinical sign for insulin resistance? Eur J Dermatol 2012 Jan-Feb;22(1):5-6. PMID 22237167.
- Eley KA, Pleat JM, Wall SA. Reconstruction of a congenital nasal deformity using skin tags as chondrocutaneous composite graft. J Craniofac Surg 2009 Mar;20(2):573-5. PMID 19305262.
- Belgam Syed SY, Lipoff JB, Chatterjee K. Acrochordon. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- El Safoury OS, Fawzy MM, Hay RM, Hassan AS, El Maadawi ZM, Rashed LA. The possible role of trauma in skin tags through the release of mast cell mediators.Indian J Dermatol. 2011 Nov;56(6):641-6.