Case Report of Vision Threatening Papilledema due to Idiopathic Intracranial Hypertension
Home / Neuro-Ophthalmology / Grand Rounds Presentations and Cases
Title: Case Report of Vision Threatening Papilledema due to Idiopathic Intracranial Hypertension
Author: Robert Henseler, 4th Year Medical Student, Rutgers University – New Jersey Medical School
CC: Headache and Blurry Vision
HPI: A 20 y/o obese woman presents with a 2-week history of blurry vision and headaches. She was originally diagnosed with a urinary tract infection and prescribed cefuroxime. After seeing her regular physician, she was referred to an ophthalmologist for her visual symptoms where optic nerve swelling on exam and visual field defects on Humphrey Visual Field (HVF) testing were detected. She also complained of neck pain and photophobia so she was sent to the emergency room to rule out the possibility of meningitis. Ophthalmology was consulted and grade 4 disc edema was noted, showing hemorrhages off the discs, tortuous vasculature, and few macular and peripheral hemorrhages. She also had visual field defects on confrontation testing, a left RAPD, and acuity of 20/100 OD and 20/80 OS. A CT and MRI were performed which suggested increased intracranial pressure. A lumbar puncture (LP) was then performed with opening pressure of 56cm H20. At the time of her first LP, 32ml of CSF were removed and closing pressure was 7cm H20. Patient had some resolution of headache and reported slightly improved vision. Her symptoms returned the next day and a repeat LP done the with 30ml of fluid removed.
Testing During Admission:
LP in Lateral Decubitus Position:
- Opening Pressure 56 cmH20
- No signs of infection
MRI Orbits:
- Flattening of the posterior globes
- Enhancement and intraocular protrusion of the optic nerve heads
- Prominent symmetric optic nerve sheath fluid and enhancement
- Mild symmetric proptosis is suggested
MRI Brain:
- No mass lesions
- No hemorrhage
CTV:
- Patent vessels proximally
- Focal narrowing at the bilateral transverse and sigmoid sinus junctions without intraluminal thrombus or evidence of external compression
- Sigmoid sinuses patent distally
The patient was then seen in the neuro-ophthalmology clinic for evaluation.
Neuro-Ophthalmologic History, Exam, and Testing Obtained Day After Admission:
Headache History:
- Located behind her eyes and wrapped around her forehead.
- Started the day following blurry vision and was a sharp pain. 9/10 in severity.
- Originally worse when laying down.
- Pulsatile tinnitus starting 4 days prior to admission.
- Intermittent visual field defects in her left eye when looking straight ahead
- Transient visual obscurations. Her left eye vision was “completely dark” for 2 days prior to admission but it came back on the day before hospital admission.
- Blurry vision in both eyes and constant binocular double vision.
- Tried ibuprofen and acetaminophen but with no relief.
- Morphine given after arrival to the ED, but also provided little to no relief.
- Now after second LP having headaches that are worse when sitting up and better with lying down.
- Patient had no history of migraines, carsickness, nausea, vomiting.
Weight History:
- High School Graduation weight: 170 pounds
- Current weight: Patient thinks 193 pounds but unsure
- Actual weight during admission was 237 pounds
- Maximum weight: Not sure but believes now is her heaviest weight
IIH Associations:
- COPD: Never smoker
- Venous thrombosis: None
- Steroids use and withdrawal: None
- Oral Contraceptive: Nexplanon implant for the past 2 years
- Vitamin A: None
- Tetracyclines: None
- Isotretinoin: None
Exam:
- EOMs were full and ortho bilaterally
- Hertel Testing 20, 20 at base 95
- Visual Acuity OD 20/70 -1, OS 20/70. No improvement with pinhole
- Pupil exam was normal except for a RAPD of 0.6 log in the left eye
- Anterior segment exam was normal
- Fundus exam showed grade 3 disc edema with boggy macula and tortuous vessels OU
Hospital Course:
Patient continued to stay in the Neuro Critical Care Unit. A lumbar drain was placed by neurosurgery after her visit to the ophthalmology clinic. Neuro-ophthalmology continued to follow the patient and it was decided that if she did not have resolution of increased ICP and vision threatening papilledema then a bilateral nerve sheath fenestration would be performed by oculoplastic surgery. Due to lack of improvement the patient underwent surgery on hospital day 3. Her surgery was performed successfully with no complications. Neuro-ophthalmology continued to follow the patient during her stay at the hospital and then manage her care following discharge on hospital day 4. She was discharged on acetazolamide 1000 mg BID to lower CSF production, gabapentin for acetazolamide induced peripheral neuropathy, and hydrocodone/acetaminophen 10/325 for pain.
4 Days after Discharge:
Interval History:
- Headaches improved, occasional headache while upright
- Transient visual obscurations: none
- Pulsatile Tinnitus: resolved
- Vision acuity subjectively improved
- Peripheral Vision: improved
- Diplopia: still had oblique diplopia
Exam:
- Visual Acuity improved to OD 20/40, OS 20/40 -1
- Left RAPD 0.6 log
- Surgical incisions clean with mild upper eyelid edema
- Anterior segment exam normal
- OD grade 3 edema with punctate hemorrhages peripapillary
- OS grade 3 edema (OS>OD) with peripapillary hemorrhage nasally
- Tortuous vessels OU
Plan:
- Continue acetazolamide 1000mg BID
- Follow up 1 week
12 Days after Discharge:
Interval History:
- Patient reports worsening symptoms beginning 5 days prior
- Symptoms include nausea, worsened supine headaches, and more pulsatile tinnitus
- Blurry and double vision subjectively worse
Exam:
- Visual acuity decreased since last visit. 20/60 OD, 20/60+1 OS.
- OD Grade 3 edema, no hemorrhages
- OS Grade 3 edema, superior resolving hemorrhage
Plan:
- Therapeutic LP now
- Increase acetazolamide to 2000mg BID
- Follow up 1 week
- If not improved will consider shunt placement
18 Days after Discharge:
Interval History:
- Visual fields are subjectively the same for her
- Blurry vision the same
- Double vision almost resolved
- Following LP last visit had improvement of symptoms for 1 day
- Pulsatile tinnitus returned
- Headache continues
- Nausea continues
- On acetazolamide 2000mg BID
Exam:
- Visual acuity improved to 20/30-2 OD, 20/30-2 OS. No change with pinhole
- Left RAPD 0.3 log
- OD grade 2 edema, no hemorrhages
- OS grade 2 edema, superior resolving hemorrhage
- Tortuous vessels OU
Plan:
- Still having significant IIH symptoms despite 2000mg BID Diamox
- Side effects almost intolerable
- Visual fields and acuity slightly improved
- Start Lasix 20mg BID trial
- Refer to neurosurgery for shunt placement due to continued IIH symptoms
- Follow up after shunt placement or with worsening symptoms
Discussion of Case:
This was a sudden onset severe case of IIH where many specialties were involved in trying to prevent papilledema induced vision loss. The important aspects of care after admission to the hospital were quick imaging (MRI of the Orbits, Brain and CT Venogram), LP in lateral decubitus, and ophthalmology consultation, examination, and HVF testing. The initially differential diagnosis for increased ICP could include a multitude of pathologic processes.
Differential Diagnosis of Papilledema and Increased ICP:
- Intracranial mass lesion, tumor or hematoma
- Cerebral edema from acute hypoxic ischemic encephalopathy, large cerebral infarction, or traumatic brain injury
- Choroid plexus papilloma causing increased CSF production
- Arachnoid granulation adhesions resulting in decreased CSF absorption
- Obstruction of venous outflow from venous sinus thrombosis or jugular vein compression
- Obstructive hydrocephalus (meningitis, cyst, or Chiari malformation)
- Idiopathic intracranial
The MRI of the orbits, brain, and spine are used to assess for many of these causes as well as the ability to show signs of increased ICP. It is also important to rule out brain herniation which would be a contraindication to LP. The CTV was performed to rule out venous sinus thrombosis. The LP in lateral decubitus position is then used to assess the opening pressure. It is also important to test for infectious causes and meningitis. Quick ophthalmologic consultation is also vital to look at the severity of papilledema and guide management. HVF testing was used to track visual field deficits resulting from papilledema and OCT was used to measure and follow the amount of optic nerve swelling. After all the testing, as well as obtaining a thorough history, the diagnosis of IIH was made with weight gain and obesity as the most likely etiology.
The rapid progression and severity of symptoms in the patient’s clinical course led to more aggressive treatment of her vision threatening papilledema. During her first 2 days in the hospital she had two LPs performed and a drain placed to remove fluid and control pressure. The decision for bilateral optic nerve sheath fenestration—while controversial due to risk of damage to the optic nerve—can be safely performed by a well-trained oculoplastic surgeon and provide significant relief to the optic nerves. Performing optic nerve sheath fenestrations unilaterally is more common. During the case, discussions were made about how best to perform optic nerve sheath fenestration while a patient has a drain. Having fluid surrounding the optic nerve allows for easier and safer surgery but increases the pressure and can cause more damage to the optic nerve. It was decided that moving forward it is best to place the drain at a height so as to maintain a pressure of 20 cmH20 a few hours prior to surgery thus allowing safe surgical approach while minimizing the risk of progressive visual damage.
Since the patient continued to have severe symptoms of increased ICP as well as minimal improvement of OCT and HVF the dose of her acetazolamide was increased to 2000mg BID at day 12 post D/C. This is a large dose and the patient was unable to tolerate the adverse effects of the medication and still continued to have symptoms of increased ICP. While not usually necessary to control optic nerve swelling and IIH symptoms, the decision was made to place a CSF shunt. This was a severe and rapid case of IIH. Aggressive medical and surgical treatment was used in order to minimize optic nerve swelling and symptoms of increased ICP. In summary, severe visual symptoms should always be addressed rapidly by an ophthalmologist as delay can lead to permanent visual deficits. Management should always be individually tailored as not all cases require the same treatment course.
Fundus Photo Right – 4 days post D/C
Fundus Photo Left – 4 days post D/C
Grade 3 papilledema OU with loss of major vessels bilaterally as they exit the disc. The left disc is more edematous than the right. Vessels are tortuous and areas of hemorrhage are seen.
OCT Right – during admission
OCT Right – 4 days post D/C
OCT Right – 12 days post D/C
OCT Right – 18 days post D/C
The edema of the right optic nerve progresses to week day 12 and then begins to resolve slightly by day 18 even though measurements are still above normal limits.
OCT Left – during admission
OCT Left – 4 days post D/C
OCT Left – 12 days post D/C
OCT Left – 18 days post D/C
Optic nerve swelling is more significant in the left eye compared to the right which corresponds to the left RAPD as well as exam findings. It is slightly improved from baseline after 2 LPs, a drain, and optic nerve sheath fenestration, but then progresses again on day 12. By day 18 after 1 week of 2000mg BID acetazolamide it is resolving slightly.
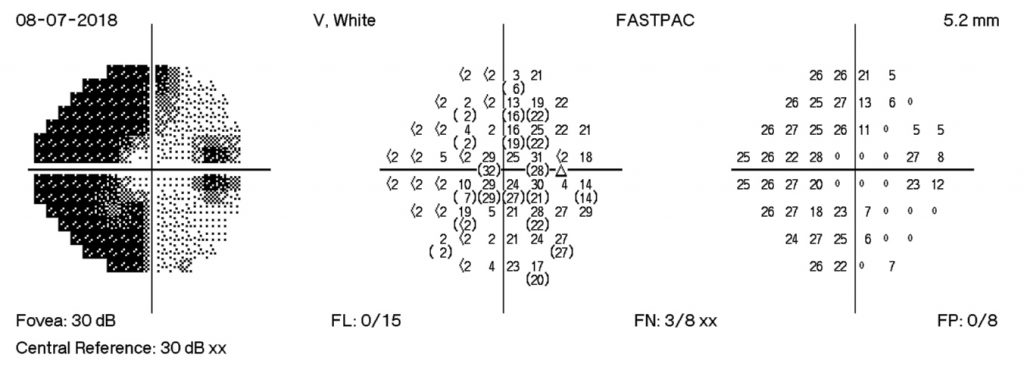
HVF Right – during admission
HVF Right – 4 days post D/C
HVF Right – 12 days post D/C
HVF Right – 18 days post D/C
The HVF on the right shows enlarge blind spots temporally and arcuate defects nasally. There is progression of visual field losses until day 12 post D/C with some improvement by day 18 post D/C. These findings correspond with patient symptoms as well as with OCT measurements.
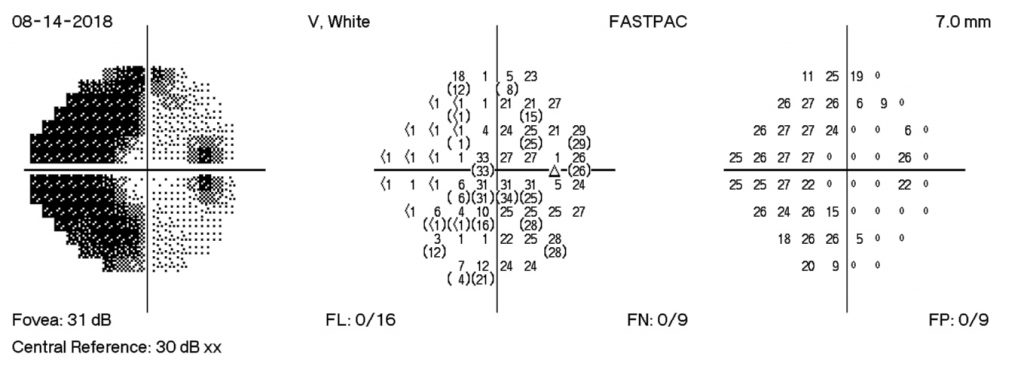
HVF Left – during admission
HVF Left – 4 days post D/C
HVF Left – 12 days post D/C
HVF Left – 18 days post D/C
The HVF on the left shows enlarge blind spots temporally and arcuate defects nasally that expand past midline temporally. There is progression of visual field losses until day 12 post D/C with some improvement by day 18 post D/C. The visual field defects are more significant in the left eye than the right eye. These findings correspond with exam findings, fundus photographs, and OCT measurements.
Identifier: Moran_CORE_25503