Susac’s Syndrome
Home / Retina and Vitreous / Other Retinal Vascular Diseases
Title: Susac’s Syndrome
Author: David F. Skanchy
Photographer: James Gilman, CRA, FOPS; Becky Weeks
Date: 9/20/2018
Keywords/Main Subjects: Susac’s Syndrome; Branch Retinal Artery Occlusion
Diagnosis: Susac’s Syndrome
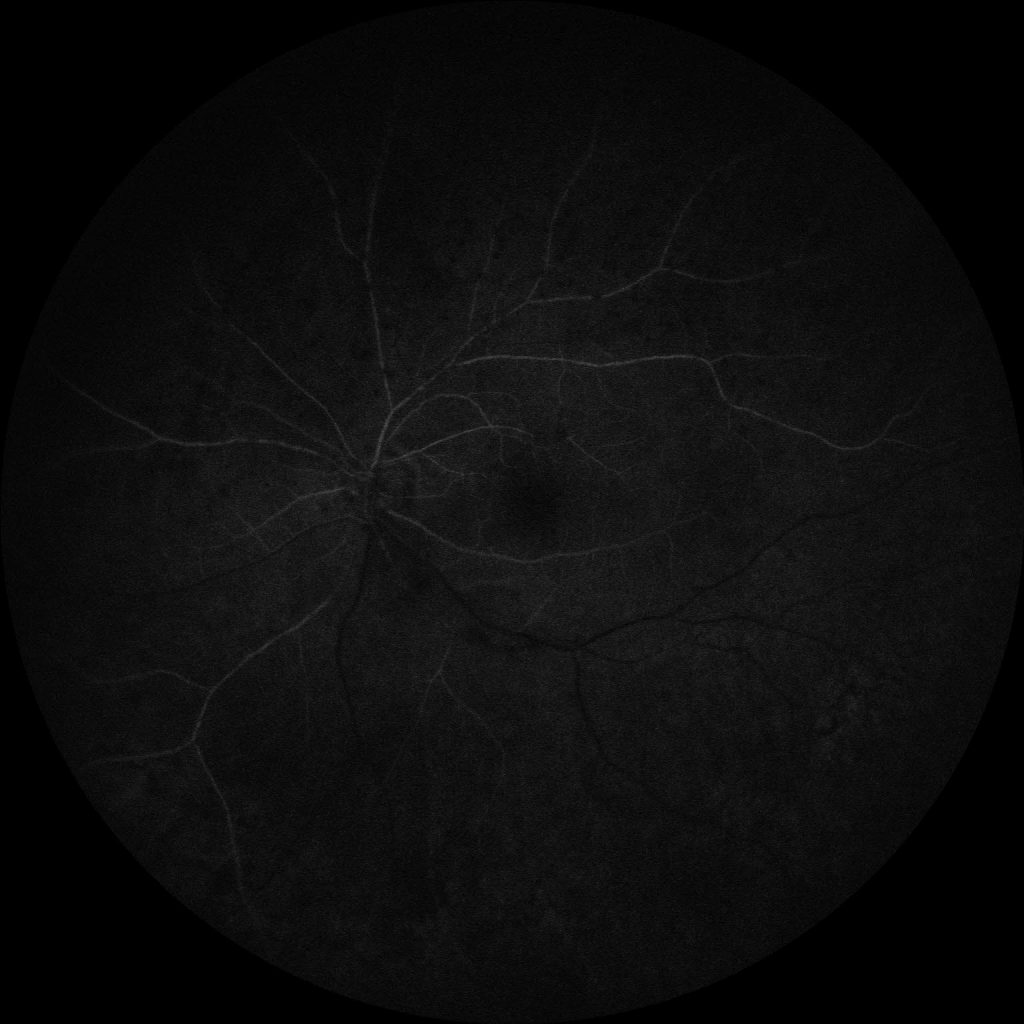
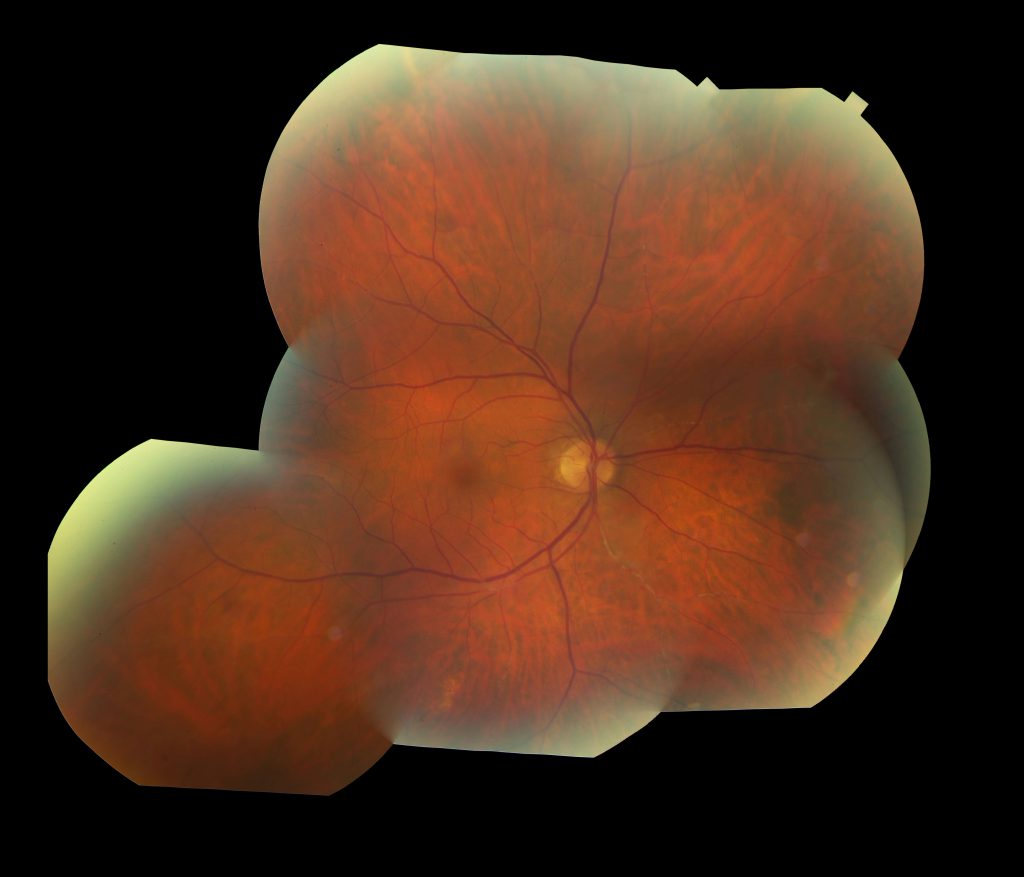
Description: A 73 year old Caucasian male presented with complaints of new onset floaters in his left eye that began 4 months prior and had been worsening over the last 3 weeks. He described it as “trying to look through a piece of lace”. He was seen by optometry and then referred to ophthalmology for concern of a possible retinal detachment, although none was noted on examination. Ophthalmology was concerned for branch retinal artery occlusions and referred the patient to a retina and uveitis specialist who performed fluorescein angiography (FA), confirming the finding of multiple branch retinal artery occlusions (Figure 1).
Past medical history was significant for a 10 year history of hearing loss requiring hearing aids. He had a history of headaches, hypertension, hyperlipidemia, smoking, and coronary artery disease with bypass surgery and mitral valve repair six years prior. The patient was also struck by lightning 20 years earlier which entered on the top right of his head and exited out of his chest.
The multiple branch retinal artery occlusions was concerning for possible Susac’s Syndrome, idiopathic retinal vasculitis-aneurysms-neuroretinitis syndrome (IRVAN), or systemic vasculitis (infectious or lymphoma associated). Around this same time the patient began getting headaches again, mostly in the left temporal/frontal region. Additionally, a significant anterior capsular cataract was seen in the left eye.
Initial workup was negative for ANA, ACE, ANCA, RPR, anti-phospholipid panel, RF, anti-CCP, and Quantiferon GOLD.
FA was consistent with a chronic process (no active inflammation) and the presence of Gass plaques (atheromatous deposits) in his left eye.
The patient was started on prednisone 60 mg with a slow taper and referred to neurology. A hypercoagulable work-up including antithrombin panel, protein C and S, and prothrombin gene mutation testing was done with only protein C being slightly elevated. A vessel wall MRI was negative. Neurology agreed that he did not have an active vasculitic process.
At this point the patient was seen by ENT who reported a decline in hearing with moderate to severe sensorineural hearing loss consistent with Susac’s Syndrome. The patient also had some difficulties remembering what he has been saying, often in the middle of a sentence. However, MRI brain, chest imaging, and echocardiogram which were all within normal limits (no vegetation with good cardiac function). Ophthalmology started the patient on mycophenolate mofetil 500 mg twice a day which was increased to 1,000 mg twice a day.
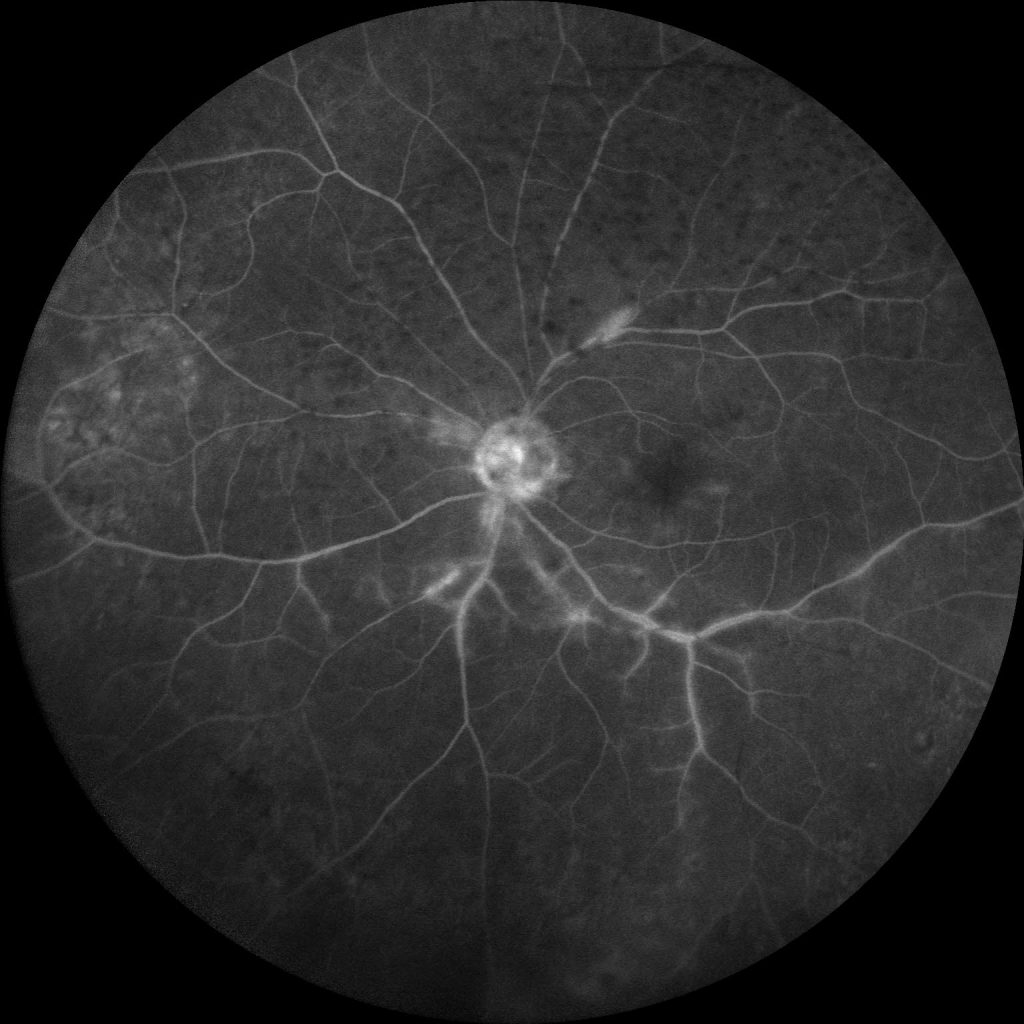
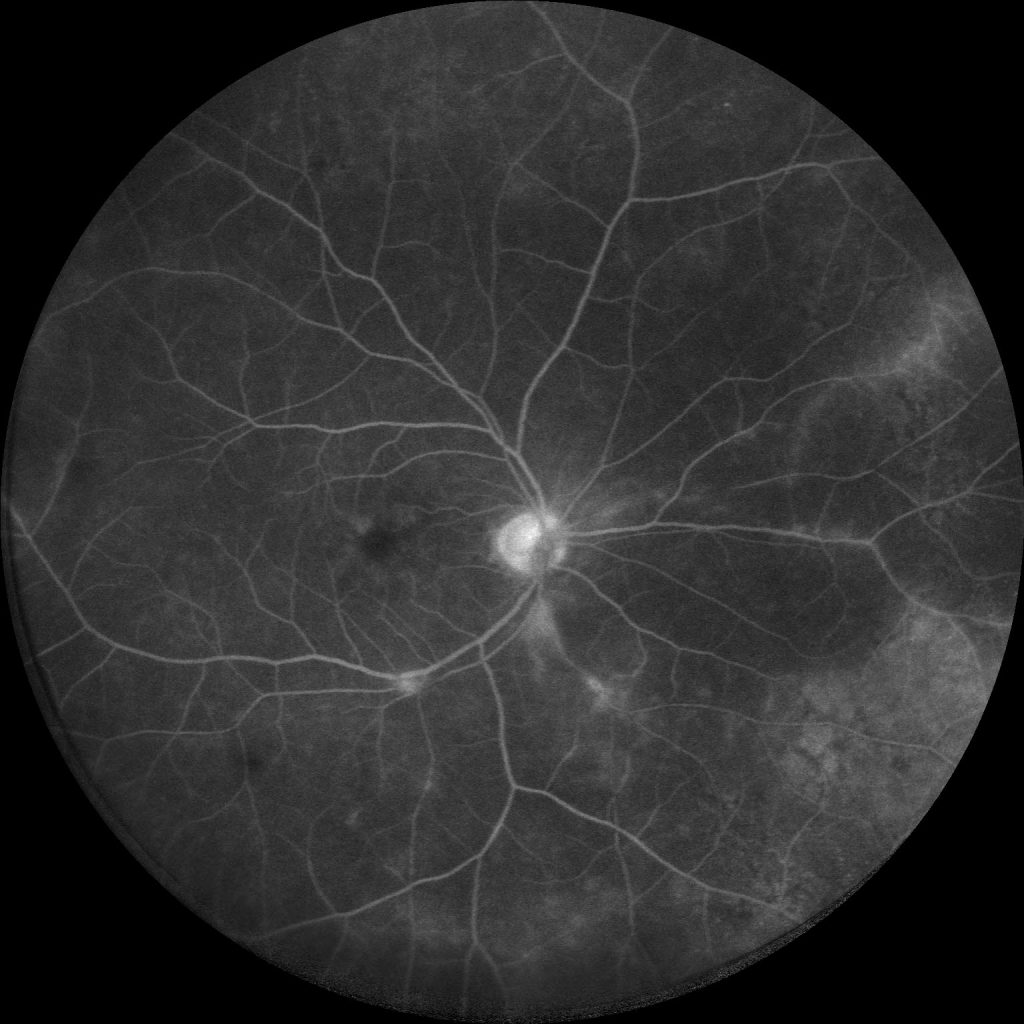
The patient received new hearing aids and showed improvement. With prednisone and mycophenolate mofetil he had dramatic ocular impro vement on FA, which showed reperfusion, no neovascularization, and improving vasculitis (Figure 2). At this time the patient is currently stable on mycophenolate mofetil 1 gm with 20/20 visual acuity in the left eye status post cataract surgery.
Summary of Case:
- Encephalopathy
- Branch Retinal Artery Occlusions (BRAO)
- Sensorineural Hearing Loss
However, the diagnosis of Susac Syndrome does not require the presence of all three findings. Three forms of Susac Syndrome have been reported and are characterized by their predominant findings. The first is characterized by encephalopathy; the second by BRAO and hearing loss, with little to no brain disease; the third by early encephalopathy with recurrent episodes of BRAO following the resolution of the encephalopathy. Other cases of Susac Syndrome have been reported by our institution highlighting the encephalopathic forms of the disease. However, this case was unique in that the initial presenting symptom that ultimately led to the diagnosis of the disease was new onset floaters. This case also presents a much older patient than is typically seen in Susac Syndrome. This presentation best falls into the second form of Susac Syndrome, with BRAO and hearing loss occurring over a more prolonged and chronic course (often 3-10 years).
Etiology/Epidemiology:
- Autoimmune. Anti-endothelial cell antibodies attack the endothelial lining of the capillaries, venules, and arterioles of the brain, retina, and inner ear.
- It has also been called retinopathy, encephalopathy, deafness associated microangiopathy (RED-M) or small infarctions of cochlear, retinal, and encephalic tissue (SICRET).
- Typically affects young women (ages 20 to 40), however, has been reported in individuals from 9 to 72 years of age.
Signs and Symptoms:
- Neurologic
- Cognitive dysfunction (memory loss, confusion, headaches)
- Gait disturbances
- Dysarthria (slurred speech)
- Psychiatric symptoms (personality changes)
- Ophthalmic
- Retinal symptoms (floaters, flashes, curtains)
- Multifocal BRAO
- Hearing
- Unilateral or bilateral hearing loss (especially mid and low frequencies)
- Tinnitus (ringing in the ear)
- Vertigo (difficulties with balance)
Diagnosis/Treatment:
- As Susac Syndrome is a rare disorder and difficult to define, the criteria for diagnosis yet to be determined.
- Some have suggested a definitive diagnosis should include brain involvement (with typical MRI lesions, “snowball”, in the corpus callosum and/or new onset headache), retinal involvement (BRAO), and vestibulocochlear involvement (new onset tinnitus, hearing loss, and/or peripheral vertigo). A probable diagnosis would include two of the three aforementioned criteria.
- The current mainstay of treatment involves corticosteroids, intravenous immunoglobulins (IVIG), and/or other immunomodulatory drugs.
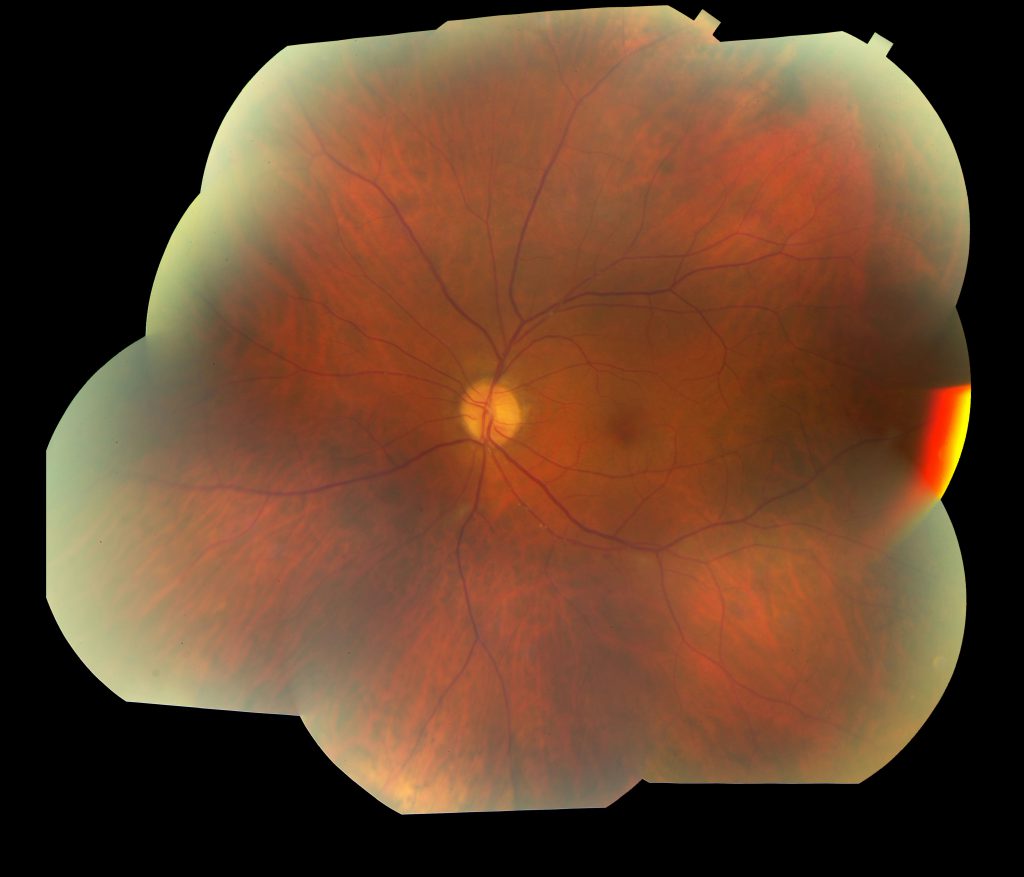
Figure 1:
Color fundus photography and FA (6/23/17) showing: Arteriole occlusions, leakage and staining of vessels in both eyes, and vitreous opacities in the left eye.
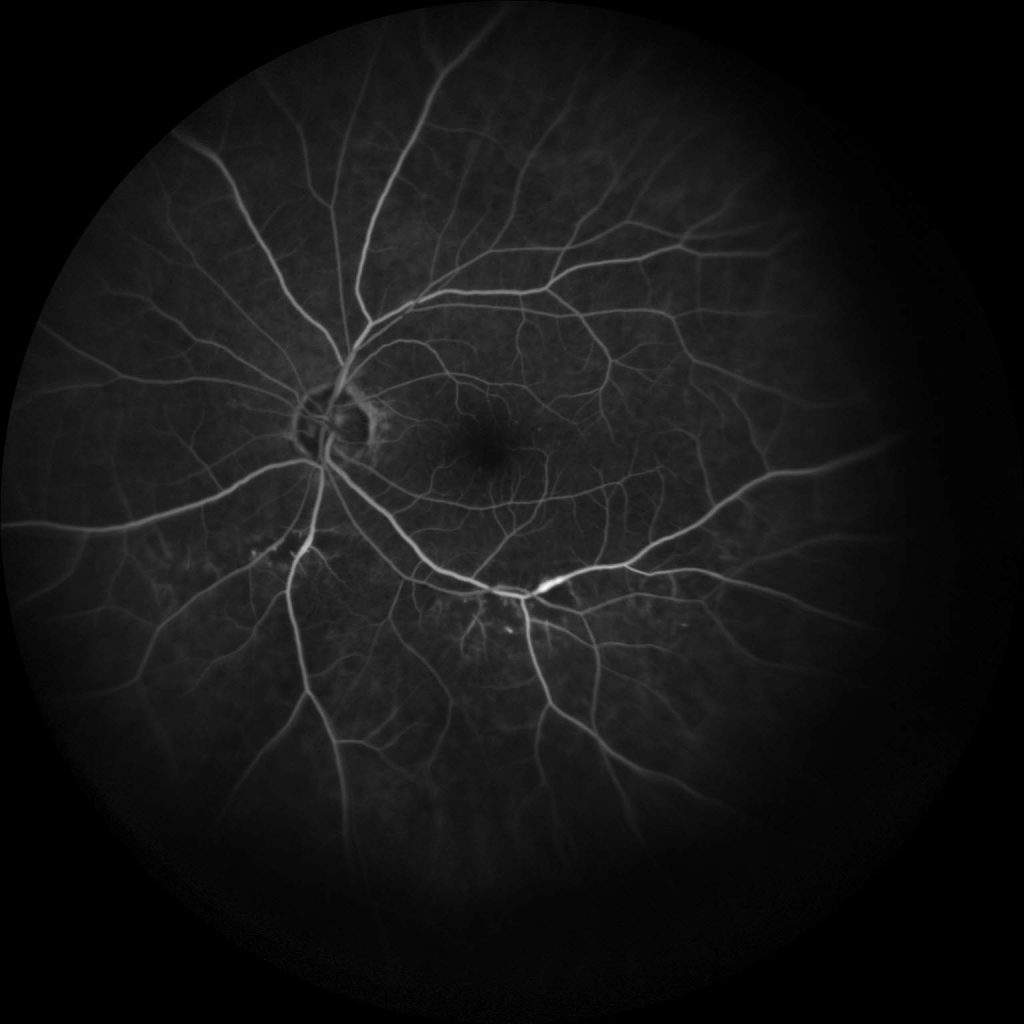
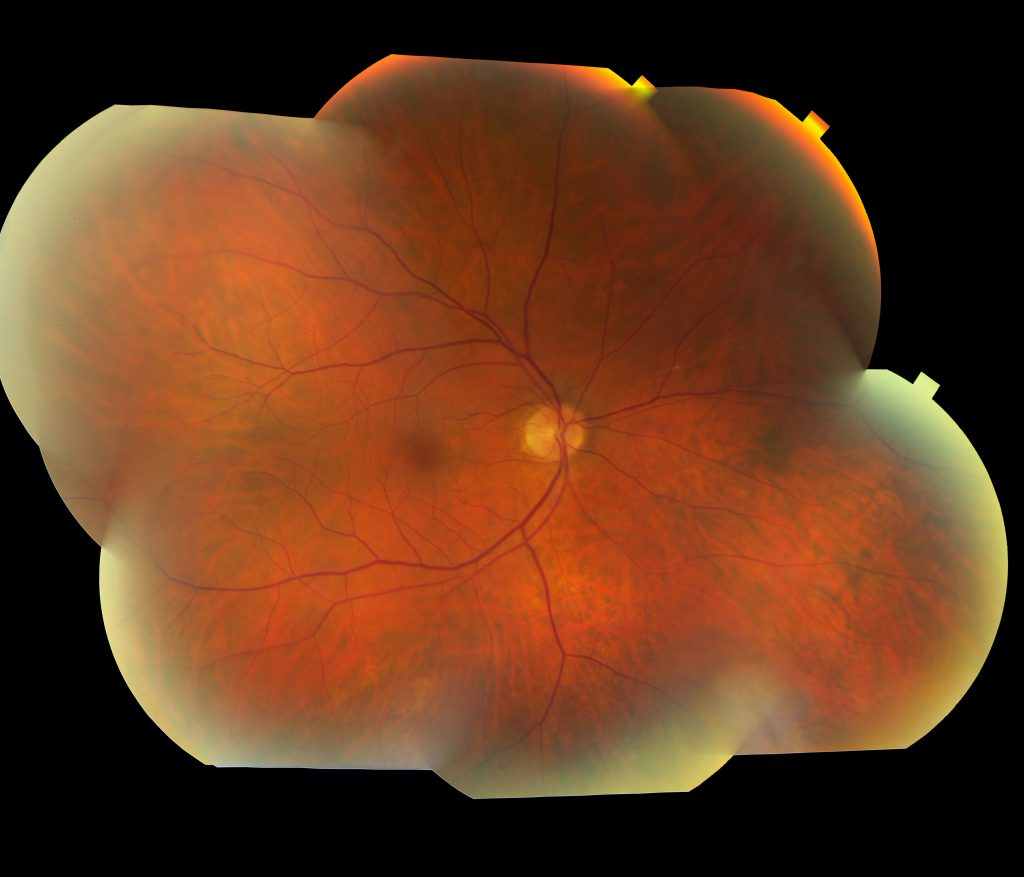
Figure 2:
Color fundus photography (10/24/17) and FA (1/29/18) showing: OD: Nasal arteriole non-filling then back filing, peripheral nonperfusion is improved, overall improvement in leakage/staining and perfusion. OS: Improvement in vascular staining and filling, a few hypofluorescent spots remain superior to arcades.
Format: Photo
References:
Kleffner I, Dörr J, Ringelstein M, Gross CC, Böckenfeld Y, Schwindt W, Sundermann B, Lohmann H, Wersching H, Promesberger J, von Königsmarck N. Diagnostic criteria for Susac syndrome. J Neurol Neurosurg Psychiatry. 2016 Dec 1;87(12):1287-95. Rennebohm R, Susac JO, Egan RA, Daroff RB. Susac’s syndrome—update. Journal of the neurological sciences. 2010 Dec 15;299(1-2):86-91. “Susac Syndrome.” Genetic and Rare Diseases Information Center. U.S. Department of Health and Human Services. Web. Accessed 19 September 2018. https://rarediseases.info.nih.gov/diseases/7713/susac-syndrome
Identifier: Moran_CORE_26651