MEWDS (Multiple Evanescent White Dot Syndrome)
Home / Retina and Vitreous / Focal and Diffuse Choroidal and Retinal Inflammation
Title: MEWDS (Multiple Evanescent White Dot Syndrome)
Author: J. Erik Kulenkamp
Photographer: James Gilman
Date: 07/10/17
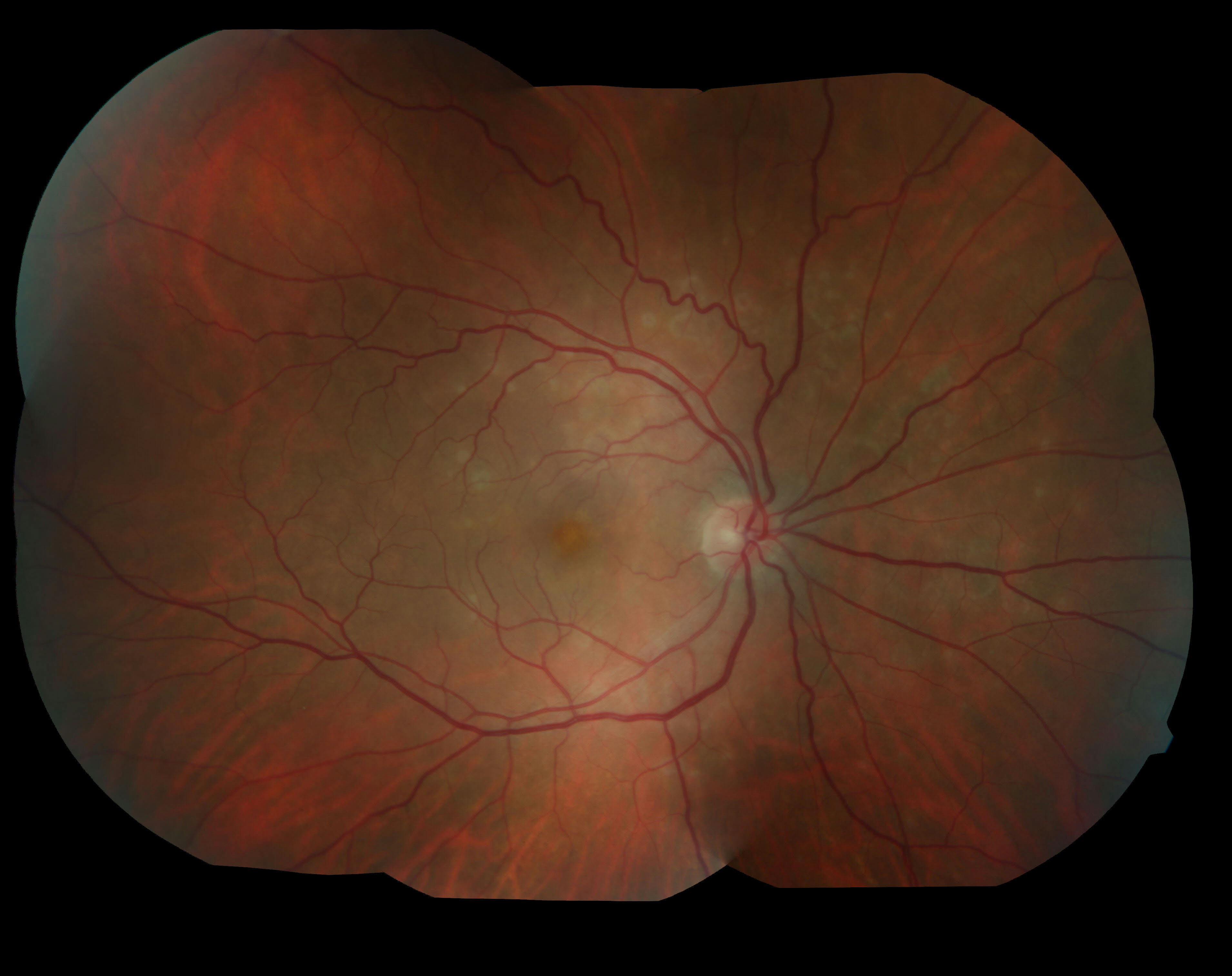
Figure 1: Montage Color Fundus Photo, Right Eye
Figure 2: Fundus Autofluorescence, Right Eye
Figure 3: Fluorescein Angiogram, Right Eye
Keywords/Main Subjects: Disorders of the Retina and Vitreous – Noninfectious Retinal Inflammation
Diagnosis: MEWDS (Multiple Evanescent White Dot Syndrome)
Description of Image: Multiple Evanescent White Dot Syndrome, or MEWDS, is a rare condition characterized by noninfectious inflammation at the level of the retinal pigment epithelium. It is part of a group of white dot syndromes that also includes acute posterior multifocal placoid pigment epithelipathy, birdshot retinopathy, multifocal choroiditis, multifocal choroiditis and panuveitis, punctate inner choroidopathy, and serpiginous choroidopathy1. MEWDS is much more common among females, especially those who are myopic, and typically appears in middle age. Patients usually present with decreased vision in one eye involving an enlarged blind spot, but they also occasionally experience photopsias. One-third of MEWDS cases are proceeded by a viral illness several weeks before becoming symptomatic2. When MEWDS is suspected, it is important to rule out neoplastic and infectious causes, which can sometimes share similar presentations. The characteristic finding on dilated fundoscopic examination (DFE) is small, intraretinal white dots in a wreath-like distribution around the macula3. The majority of patients improve within 2-6 weeks without steroid treatment, although the occasional individual will have a persistently enlarged scotoma2.
A 48 year old myopic female presented with one week of an enlarged blind spot. She recalls that parts of words were missing from her vision in her right eye and that the area of missing vision was surrounded by blurriness. She was born in Argentina, but denied recent travel, fevers, weight loss, shortness of breath, recent illness, pets, STI’s, or IV drug use. Visual acuity in the right eye was 20/80 -1, down from 20/50 -1 six months prior, and 20/20 in the left eye. On DFE, numerous white dots were observed in a wreath-like distribution around the macula, ranging 200-300 microns in size. These dots can be seen in Figure 1, which demonstrates the classic appearance of MEWDS in a montage color fundus photo of the right eye. The optic nerve and disc appear normal, as do the vessels, but there is foveal granularity in the macula. The white dots are densest emanating from the optic nerve. Figure 2 is a fundus autofluorescence (FAF) photo of the same eye, illustrating a multitude of hyperfluorescent dots surrounding the optic nerve and extending to encompass the macula. The extent of retinal involvement, especially nasally, is much more apparent in the FAF. Figure 3 demonstrates a fluorescein angiogram with hyperfluorescence in a similar pattern to the FAF, which remains notable in the late phase. Again, the wreath-like distribution with greatest density near the optic nerve is visible. 30-2 Humphrey Visual Field correlated with the patient’s history of an enlarged blind spot in the right eye. Each study was performed in the left eye as well, but all were unremarkable. Additional workup including CBC, CMP, ESR, CRP, FTA-ABS, ACE, lysozyme, quanterferon gold, and CXR were within normal limits, making MEWDS the presumptive diagnosis. On follow up ten days later, the patient reported improved blurriness and resolution of her scotoma without treatment, and OD visual acuity improved to 20/70 -2.
References:
- Raven ML, Ringeisen AL, Yonekawa Y, Stem MS, Faia LJ, Gottlieb JL. Multi-modal imaging and anatomic classification of the white dot syndromes. Int J Retina Vitr. 2017;3:12. doi:10.1186/s40942-017-0069-8.
- McCannel, Colin. 2017-2018 Basic and Clinical Science Course: Retina and Vitreous: American Academy of Ophthalmology; 2017.
- Bagheri N, Wajda BN, Calvo CM, Durrani AK, Friedberg MA, Rapuano CJ. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. Seventh edition. Philadelphia: LWW; 2016.
Identifier: Moran_CORE_24094
Faculty Approval by: Griffin Jardine, MD
Copyright statement: Copyright J. Erik Kulenkamp, ©2017. Please see terms of use page for more information.