Cornea
Home / Ophthalmic Pathology / Cornea
Normal Cornea


6.01 Normal


6.02 PAS Stained Bowman’s does not stain because it is
not a true basement membrane (BM)


6.03 Magnified Cornea
- Overall
- 5 Layers: Epithelium, Bowman’s membrane, Stroma, Descemet’s membrane, Endothelium
- Diameter: 11-12 mm horizontally, 9-11 mm vertically
- About 550 microns thick centrally and 650 microns peripherally
- Epithelium:
- 5-7 cells thick, non-keratinized stratified squamous
- Attached to thin BM by hemi-desmosomes and filaments
- BM seen with PAS stain
- Derived from surface ectoderm
- Bowman’s Membrane:
- Acellular, irregularly arranged collagen fibrils
- Does not regenerate
- Not a basement membrane, not PAS+
- 8-14mm thick
- Stroma:
- 90% of total thickness
- Crystalline ordering of collagen fibers for clarity
- “Ground substance” coats collagen fibrils and allows correct spacing
- Collagen producing keratocytes, collagenous lamellae, proteoglycan ground substance
- Posterior stroma adheres to underlying Descemet’s
- Descemet’s Membrane:
- Produced by endothelium
- Continually thickening through life
- True basement membrane of type IV collagen
- PAS +, does regenerate. TEM shows banded and non-banded layer
- Endothelium:
- Monolayer, neural crest derived, does not readily regenerate
- Pumps water from cornea to maintain clarity-deturgescence
- Number of cells decreases throughout lifetime. Remaining cells flatten and spread
- Produces Descemet’s throughout lifetime
- Tight junctions between cells, hexagonal
Congenital Abnormalities
- CHED (Congenital hereditary endothelial dystrophy)–2 histologically similar forms
- Autosomal Recessive
- More common than autosomal dominant
- Present at birth
- Stable
- Frequently associated with nystagmus
- Blue-white cornea
- Pachymetry is 2-3 times normal thickness
- Stroma opacified
- 20p13 loci
- Autosomal dominant
- Appears in 1st-2nd year of life
- Similar appearance
- Zero nystagmus –occurs after fixation develops
- May have pain/photophobia
- Both are similar histo-pathologically and have the features of
- Stromal edema
- Thickened Descemet’s
- Atrophic endothelium
- Degeneration of endothelium at 5th month gestation
- Zero systemic abnormalities
- Autosomal Recessive
- Peters Anomaly:


6.04 Slit lamp


6.05 PAS stain


6.06
-
- Anterior segment dysgenesis
- Neural crest doesn’t migrate properly
- Bilateral and sporadic, can be autosomal dominant or recessive
- Bilateral central corneal opacities, absormal stroma, and local absence of endothelium and Descemet’s
- May see cornea plana
- Curvature of the cornea is flattened
- May see sclerocornea
- Peripheral corneal opacification and vascularization
- Can see internal ulcer of von hippel
- Central or paracentral portion of Descemet’s
- At edges of defect iris strands adhere to posterior corneal surface
- Endothelium and Descemet’s are absent centrally
- Posterior Keratoconus: (internal ulcer of von Hippel)
- Thinning and hazy cornea from A/C side
- Descemet’s and endothelium intact
- Females>males, spontaneous, non-progressive
- Astigmatism and amblyopia possible
- Crater-like corneal depressions
- Stromal collagen disarray of overlying collagen in stroma
- Bowman’s maybe absent centrally
- Congenital Corneal Staphyloma
- Scarred cornea and limbal tissue
- Sclerocornea:
- Non -progressive, non -inflammatory
- Poorly defined limbus
- 90% bilateral
- 50% sporadic. Also AD and AR (more severe)
- Cornea plana 80%
- Cornea appears white
- Increased numbers of collagen fibrilsof various diameters, decreasein diameters of collagen fibrils from the anterior to the posterior layers, and thin Descemet’s membrane
- May involve whole cornea or peripheral with superficial or deep vascularization
Congenital Corneal Staphyloma-scarred cornea and limbal tissue.
Inflammation
- Infectious keratitis
- Caused by many microbial agents
- Can lead to corneal necrosis, ulceration, and perforation
- Bacterial Infection:


6.07 External photo of bacterial ulcer


6.08 Corneal perforation from a
bacterial ulcer


6.09 magnification Inflammatory cells after corneal perforation
-
- Usually requires disruption of epithelium: CTL wearer, trauma, etc.
- S. Areus, S. pneumonia, P. aeruginosa, Enterobacteriaceae
- Gram stain and culture
- Scrapings will show neutrophils with necrotic debris
- Herpes Simplex Virus:


6.10 Slit lamp photo Dendrite


6.11 Herpes Simplex Keratitis


6.12 Stroma herpes simplex


6.13 Higher magnification


6.14 Corneal scrapings
-
- Arborizing dendrites
- Granulomatous reaction at Descemet’s membrane with stromal hepatitis
- Giemsa shows intracellular inclusions
- May have giant cells posteriorly
- Interstitial keratitis possible
- Chronic inflammatory cells and blood vessels between stroma lamellae
- Epithelium denuded in center, scrape at edge not center
- Post-herpetic neurotrophic keratopathy
- Corneal stroma void of keratocytes
- Fungal:


6.15 External photo


6.16 Gomori Methenamine-Silver (GMS) stained ulcer
-
- Usually from trauma from plant or vegetable matter, CL wear, topical steroid use
- Penetratesintact corneaand extendinto the anterior chamber
- Aspergillus, candida, fusarium (molds most important)
- Gomori-methamine silver (GMS) stains fungi silver/black
- Acanthamoeba:


6.17 External photo


6.18 Gridley stained cornea


6.19 Electron Microscopy of Acanthamoeba
-
- Contact lens wearer or hot tubs
- Chronic non-healing corneal ulcer
- Cysts stains silver on Gridley stain, but may be visible on H and E stain
- Ring infiltrate possible
- Culture on non-nutrient blood agar with E. coli overlay
- Can invade corneal nerves
- FB: granulomatous reaction
- Noninfectious keratitis
- Autoimmune diseases, topical medication toxicity
- Absence of organisms
- Interstitial keratitis
- Non-suppurative inflammatory cells infiltrate of the inter-lamellar spaces of the corneal stroma with vascularization, sparing endothelium
- Overlying epithelium intact
- Immunologic response to infectious microorganisms or antigens
- Congenitalsyphilis most common causebut also m.tuberculosis, m.leprae, b.burgdorferiand EBV
- chronic interstitial keratitis-cornealendothelium produces excess BM
- Syphilis:
- Non-suppurative inflammation of stroma with sparing of endothelium
- Stromal ghost vessels devoid of erythrocytes with surrounding stromal fibrosis and variable degree of chronic inflammation
- Bowman’s and Descemet’s intact
- May have guttae like features
- Infectious pseudocrystalline keratopathy:
-
- Lon-term corticosteroid therapy
- Usually along suture track or surgical wound
- Viridans streptococci most commonbacteria, mycobacteria and fungi
- Crystalloid clinical appearance of opacity
- Colonies within inter-lamellar spaces of stroma
- Stain depends on organism
Degenerations
- Salzmann nodular degeneration:
-
- Non-inflammatory corneal degeneration
- Grey-white of blue-white lesions-central/paracentral
- Zero Bowman’s layer, nodules of basement membrane-like material
- More common in middle-aged women
- Associated with blepharitis
- Variably thick epithelium and replacement of Bowman’s layer with disorganized collagenous tissue
- Usually in area of previous corneal injury
- Band Keratopathy:


6.22 External photo


6.23 External Photo


6.24 Alizern red stained cornea
-
-
- Calcium deposition in epithelial BM, Bowman’s, and stroma. Typically sign of chronic inflammation
- Basophilic on H and E
- Alizarin red or von Kossa stains calcium
- Caused by systemic hypercalcemia, prolonged inflammation, trauma
- Typically in inter-palpebral zone sparing peripheral cornea
- Actinic Keratopathy: (spheroidal degeneration)
- Solar damage
- Oil droplet appearance in superficial stroma
- Similar pattern to band keratopathy
- Aggregates of translucent golden-brown spheroidal deposits in the inter-palpebral superficial cornea
- Bilateral, more common in males
- Basophilic globules beneath epitheliumin bowman layer and anterior stroma
- Stains black forelastin like verboeff-van gieson
-
- Pannus:


6.25 Pannus


6.26 Pannus with Calcium
-
- Fibrovascular growth between epithelium and Bowman’s
- May occur under band keratopathy or in inflammatory setting
- Seen in chronic corneal edema or prolonged corneal inflammation
- Bullous Keratopathy:
-
- Sequelae of chronic corneal-edema
- Occurs after PEIOL, but less common now with better tools and techniques
- Can initially see “ghosting” or pallor of basal side of epithelial cells
- Epithelium separates with micro cyst above Bowman’s
- BM may thicken
- Induced by endothelial cell loss leading to corneal decompensation
- Arcus Senilis:


6.28 External photo


6.29 Oil Red O stain
-
- Cholesterol stain
- Stains with oil-red-O deposition in stroma
- Clear zone at limbus
- Spontaneous Descemet’s Breaks
- Deposits in a diffusion pattern from limbus, shaped like hour glass more lipid anterior in stroma and posterior then thins out in center
- Common finding-doesn’t signify high lipid
- Keratoconus:


6.30 Munson’s sign


6.31 Slit lamp photo




6.33 Hydrops 2/2 Keratoconus PAS stain
-
- Non-inflammatory condition-usually bilateral
- Non-inherited, young girls
- Thinned central cornea
- Breaks in descemets with possible hydrops
- Iron peripherally in epithelial cells (Fleisher ring)
- Epithelium often cauterized during corneal transplant; can note “sizzle” artifact in central cornea
- Terrien’s marginal degeneration:


6.34 Terrien’s marginal degeneration
-
- Peripheral corneal stromal thinning
- Limbal lesion that spreads circumferentially
- Slow growing
- Corneal neovascularization, opacification, and lipid deposition
- Epithelium intact, Bowman’sabsent, breaks in Descemet’s
- Pellucid marginal degeneration
- Bilateral, peripheral inferior thinning
- Involved cornea has no scarring, infiltration, or vascularization
- Atypical form of keratoconus
- Delle
- Corneal thinning caused by localized area of stromal dehydration
- Break in tear film layer caused by elevation of surrounding structures
- Meesmann’s Dystrophy:


6.35 Slit lamp photo


6.36 Peculiar substance under epithelium and Bowman’s
-
- Autosomal dominant, 1st or 2nd year of life
- Peculiar substance in epithelial cells, thickened BM, and round structures multiple dots underneath
- Recurrent erosions
- Ries-Buckler:


6.37 Slit lamp photo


6.38 Ries-Buckler
-
- Autosomal dominant, Bowman’s replaced by sheet-like layer of granular deposits
- Stain red with Masson trichrome and immune-react with anti-tgfb1 antibodies
- Recurrent erosions
- Sub-epithelial honeycomb pattern
- Map-dot Dystrophy:


Slit lamp photo


6.40 Periodic acid-Schiff (PAS)
-
- Recurrent erosions
- Dysfunctional BM does not stick to epithelium
- Rib-like intraepithelial extensions of basal laminar material
- Basement membrane extends abnormally into epithelium
- Thickened BM-may extend into epithelium microcysts and abnormal epithelium resemble fingerprints
- Thiel-behnke
- “Saw-tooth pattern”
- Solitary flecks or irregularlyshaped scatteropacities at the level of bowman’slayer thatprogresses to symmetric sub-epithelial honeycomb opacities
- Curly collagen fibers 10nm diameter
Medication
- Amiodarone: Whorl-like keratopathy
- Lysosomal deposits in basal epithelium also chloroquine, indomethacin, chlorpromazine
Corneal Stromal Dystrophies
(Mnemonic to remember these dystrophies)
Marilyn Monroe Always Really Gets Her Man In LA County
Macular Mucopolysaccharide Alcian blue Recessive Granular Hyaline Masson’s trichrome Lattice Amyloid Congo red
- Macular Dystrophy: ch 16q (recessive)


6.41 External photos


6.42 Alcian blue stained cornea
-
- Entire cornea to limbus involved
- Hazy cornea in between opacities
- Monopoly-saccharide deposits intra and extracellularly of stroma and endothelium
- Stains with Alcian Blue
- Keratin sulfate and dermatan sulfate abnormalities
- Granular Dystrophy:
-
-
- AD, Central cornea involvement, Chr5q
- Hyaline granular deposits in stroma separated by clear intervening stroma
- Hyaline stains red with masson-trichrome
-
- Lattice Dystrophy:


6.45 Slit Lamp photo


6.46 Congo-red stain


6.47 Birefringenece under polarized light
-
- Hazy stroma, retractile lines chr5q
- Fusiform amyloid deposits in anterior stroma and Bowman’s layer
- *More frequent recurrence after PKP
- Apple green birefringence with cross polarized light
- Stains orange with Congo-red
- Avellino:
- Features of granular and lattice chr5q
- Hyaline and amyloid deposits.
- Fuchs Dystrophy: female>male
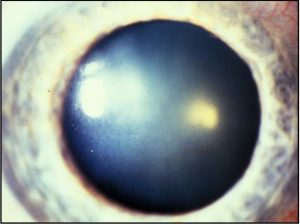

6.48 Slit lamp photo


6.49 Fuch’s dystrophy
-
- Abnormal endothelial cells lay down more Descemet’s membrane and then endothelial cells eventually die off
- Guttae in Descemet’s (diffuse thickening)
- Sparse to absent endothelial cells
- Butte-like concretions of Descemet’s noted centrally/paracentrally
- Whereas, Hassel-Henley warts are butte-like concretions of Descemet’s in far periphery attributed to age-related changes
- Common cause of bullous keratopathy
- Beaten metal appearance
- Posterior polymorphous corneal dystrophy
- AD, progressive
- Asymmetric opacities in Descemet’s
- Nodular, vesicular railroad track like lesions
- Associated with corneal edema, peripheral iridocorneal adhesions, and IOP elevation
- Descemet membrane thickened, multi-laminated with focal nodular and fusiform excrescences
- Fabry’s Disease
- X-linked recessive
- Caused by Alpha-galactosidase deficiency
- Whorl-like epithelial corneal opacities “Cornea verticillata”
- Tortuous retinal vessels
- Lipid inclusions present in corneal epithelium, in lens epithelium, and endothelial cells of all organs
Pigment Deposits
- Krukenberg Spindle:
- Pigment dispersion syndrome
- Melanin in ECs and on posterior surface
- Vertical band of melanin phagocytosed by endothelium
- Pigment released after exercise or pupil dilation
- If unilateral, trauma is the cause
- Blood staining:
-
-
- Stains with intact endothelium if very high IOP
- Low IOP stain with hemoglobin and iron mostly seen in stroma
- Amorphous globules and tiny round spheres and rods seen between k lamellas, keratocytes and Bowman’s
-
- Iron lines: basal layer of epithelium, Prussian blue stain
- Fliesher’s ring:


6.52 Fliesher’s ring in Keratoconus
-
- Deposition of iron in epithelium seen with keratoconus
- Ferry’s line
- Deposition of iron in epithelium seen with filtering bleb
- Stocker’s line
- Deposition of iron in epithelium seen in ptergyium
- Hudson-Stahli
- Deposition of iron in epithelium seen in palpebral fissure
- Kayser-Fleischer
- Copper line in peripheral Descemet’s
Neoplasms
- Neoplasms of cornea are very rare
- Bowman’s acts as a barrier to extension. More often extension from conj.
References
Rosa, Robert H., ed. Ophthalmic pathology and intraocular tumors. American Academy of Ophthalmology, 2018.
Yanoff M, Fine BS. Ocular Pathology, A Text and Atlas. Lippincott Williams & Wilkins; 1989.

















