Glaucomatous Cupping
Home / Basic Ophthalmology Review / Optic Nerve
Title: Glaucomatous Cupping
Author: Tanner Ferguson, 4th year medical student, University of South Dakota Sanford School of Medicine
Glaucoma is a term used to describe damage to the optic nerve characterized by a progressive loss of retinal ganglion cells (RGCs). Although intraocular pressure is a proven, modifiable risk factor for the disease, elevated intraocular pressure is not sufficient for a diagnosis1,2. When damage occurs in glaucoma, changes can be detected structurally and/or functionally. It is separated into open angle versus closed angle types, as well as primary and secondary. This article primarily focuses on primary open angle glaucoma (POAG). Glaucoma is a multifactorial disease process and this overview will provide a summary on the modifiable risk factors and signs/symptoms that suggest further evaluation. It is important to identify and manage these risk factors because glaucoma remains the world’s 2nd leading cause of blindness.3
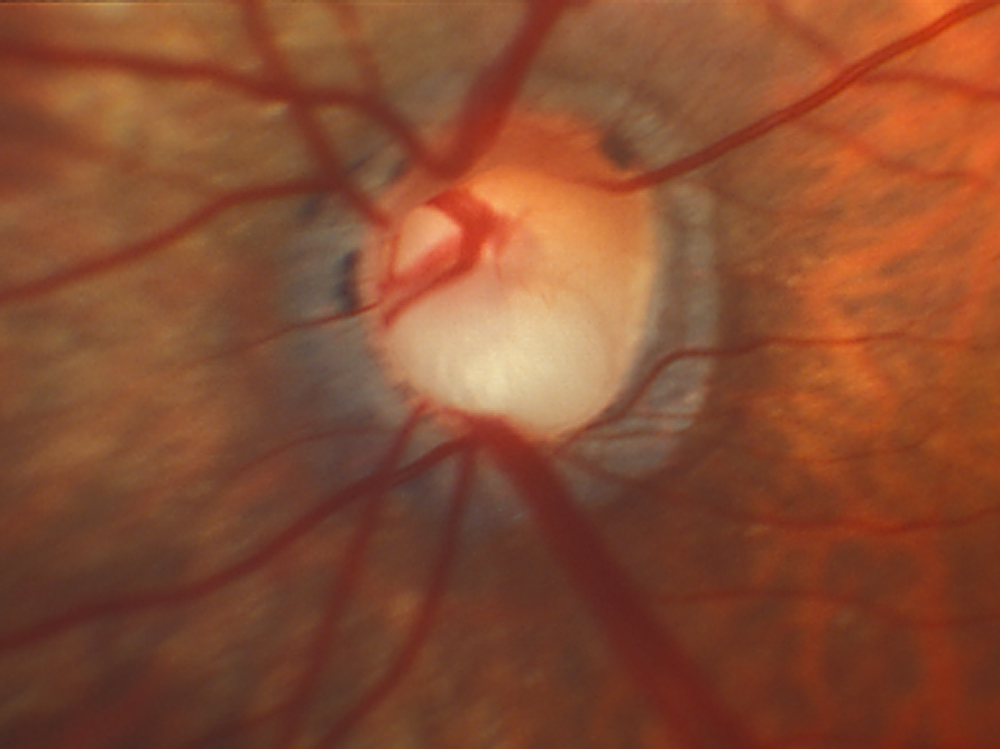
In the optic nerve, there is a physiologic disk and an indentation absent of neural tissue known as the optic cup. In glaucomatous nerve damage, the retinal nerve fiber atrophies as fibers die and the cup increases in size. To monitor progression, clinicians track the cup-disc ratio and compare to age-matched normal values.4
Risk Factors for Open Angle Glaucoma
If you suspect a patient is at risk for glaucoma, there are numerous risk factors to consider5-7, some of which are listed below:
- Family history of glaucoma
- Sleep apnea
- Blood pressure medications at night (nocturnal hypoxia)
- Diabetes mellitus, type 2
- Chronic anemia
- Systemic medications (eg, steroids)
- Carotid disease
- Phosphodiesterase inhibitors (eg, sildenafil)
- Low CSF pressure
It is critical to screen for sleep apnea or other causes of nocturnal hypoxia (such as using blood pressure medications at night) because these are easily managed with CPAP or by modifying medication timing. Numerous reports have suggested nocturnal hypoxia to be a risk factor for glaucoma progression.8,9
Symptoms
Glaucoma is typically a silent, progressive condition that is often asymptomatic until significant damage has occurred10. Studies have reported that visual field deficits are not present until a significant amount of nerve fiber layer loss has occurred11. When visual symptoms do occur, patients often have a “tunneling” of vision where peripheral vision is often affected first. Unfortunately, once noticeable vision loss has occurred the disease is likely in its advance stages. Thus, if you suspect a patient has early signs of glaucoma or has significant risk factors, it is crucial to encourage patients to seek further evaluation from their eye care provider. The vision loss is most often a very slow, smoldering, progressive process that presents later in life but not infrequently a patient may have unusually high intraocular pressures or secondary glaucoma which can cause more rapid vision loss—once again emphasizing the importance of screening and appropriately referring patients. Acute angle closure has a much different presentation, is typically painful with blurry vision and causes often very high intraocular pressures that can rapidly damage the optic nerve/retinal ganglion cells. We have included several pictures below to demonstrate the appearance of glaucomatous cupping of the optic nerve.
Images:
References
- Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120(10):1268-1279.
- Wolfs RCW, Borger PH, Ramrattan RS, et al. Changing Views on Open-Angle Glaucoma: Definitions and Prevalences—The Rotterdam Study. Investigative Ophthalmology & Visual Science. 2000;41(11):3309-3321.
- Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. British Journal of Ophthalmology. 2006;90(3):262-267. doi:10.1136/bjo.2005.081224.
- Burgoyne CF, Downs JC, Bellezza AJ, Suh J-KF, Hart RT. The optic nerve head as a biomechanical structure: a new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog Retin Eye Res. 2005;24(1):39-73. doi:10.1016/j.preteyeres.2004.06.001.
- Tielsch JM, Katz J, Singh K, et al. A population-based evaluation of glaucoma screening: the Baltimore Eye Survey. Am J Epidemiol. 1991;134(10):1102-1110.
- Leske MC, Connell AMS, Wu S-Y, Hyman LG, Schachat AP. Risk Factors for Open-angle Glaucoma: The Barbados Eye Study. Arch Ophthalmol. 1995;113(7):918-924. doi:10.1001/archopht.1995.01100070092031.
- Prum BE, Rosenberg LF, Gedde SJ, et al. Primary Open-Angle Glaucoma Preferred Practice Pattern(®) Guidelines. Ophthalmology. 2016;123(1):P41-P111. doi:10.1016/j.ophtha.2015.10.053.
- Tielsch JM, Katz J, Sommer A, Quigley HA, Javitt JC. Hypertension, Perfusion Pressure, and Primary Open-angle Glaucoma: A Population-Based Assessment. Arch Ophthalmol. 1995;113(2):216-221. doi:10.1001/archopht.1995.01100020100038.
- Leske MC, Wu S-Y, Hennis A, Honkanen R, Nemesure B, BESs Study Group. Risk factors for incident open-angle glaucoma: the Barbados Eye Studies. Ophthalmology. 2008;115(1):85-93. doi:10.1016/j.ophtha.2007.03.017.
- Sommer A, Katz J, Quigley HA, et al. Clinically detectable nerve fiber atrophy precedes the onset of glaucomatous field loss. Arch Ophthalmol. 1991;109(1):77-83.
- Miki A, Medeiros FA, Weinreb RN, et al. Rates of retinal nerve fiber layer thinning in glaucoma suspect eyes. Ophthalmology. 2014;121(7):1350-1358. doi:10.1016/j.ophtha.2014.01.017.
Identifier: Moran_CORE_23937