How to Assess Whether a Globe is Ruptured
Home / Basic Ophthalmology Review / Trauma
Title: How to Assess Whether a Globe is Ruptured
Author: Johnny Lippincott, 4th Year Medical Student, University of Mississippi Medical Center
Location: Medical Student Education Outline > II. Anatomical Approach to Eye Disease > Trauma > 2. How to assess whether a globe is ruptured
Text:
Introduction: An open globe or ruptured globe is an eyeball with a full-thickness defect in part of the eye’s wall, and is a true ophthalmic emergency. “Full-thickness” means all layers of the eye are disrupted. An open globe therefore allows communication between the eye’s interior and the environment. The danger of this communication is two-way: the eye’s internal contents can extrude, and environmental factors (e.g., pathogens) may enter.
If there is any concern that a patient may have an open globe, the top priority is avoiding further damage to the eye. This means special precautions must be taken immediately to assess whether this is the case. Until the integrity of the globe is confidently established, do not place external pressure of any sort on the eye of concern. Doing so can squeeze ocular contents through the defect and possibly cause permanent loss of vision or loss of the eye itself. Do not: patch the eye, measure intraocular pressure (e.g., with a Tonopen®), or allow the patient to rub the eye.
History
Patients may present with an open globe after various forms of trauma, from work- and sports-related injuries to falls and motor vehicle accidents. Particularly important history includes:
- Elicit possible mechanisms: was there a penetrating/perforating injury (e.g., BB gun shot), metal on metal contact without safety glasses or blunt trauma (e.g., racquetball)?
- Determine if there is potentially a foreign body based on the mechanism.
- Ask whether the patient has any prior history of eye surgery or trauma.
- Determine tetanus immunization status.
- Ask when the patient last ate or drank and instruct the patient to stop eating or drinking given they may likely need urgent surgery.
Signs of an Open Globe
A simple penlight is useful in grossly assessing the integrity of the globe.

Figure 1: Prolapsed iris through a corneal laceration with a very irregular pupil visible retina through the pupil. The conjunctiva is boggy and the entire globe appears deflated or slightly collapsed or simply “not round.”
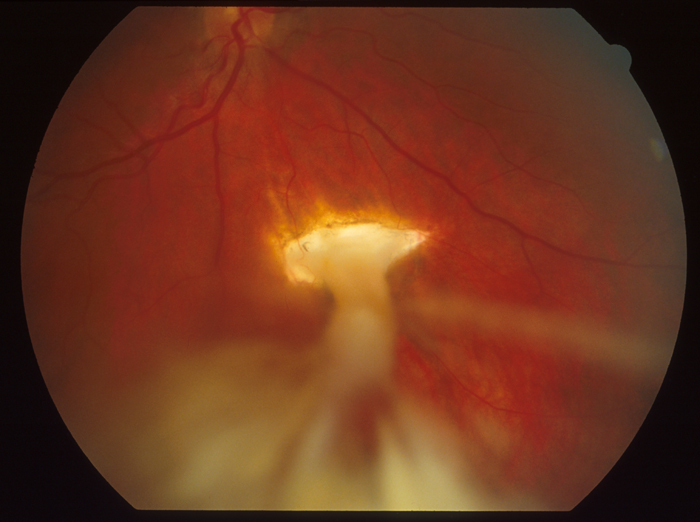
Image 2: Fundus photo of an inferior choroidal rupture versus scleral rupture with a vitreous tracking to the wound.
Pathognomonic signs:
- Full-thickness laceration(s) of the cornea or sclera
- Prolapse of intraocular contents (e.g., uveal tissue like the iris or ciliary body)
- Positive Seidel test (especially useful for known defect of unknown depth)
Three necessary tools for this test are 1) anesthetic eye drops (e.g., proparacaine HCl 0.5%), 2) fluorescein strip, and 3) cobalt blue light source with slit lamp/magnification. After numbing the eye with drops, gently paint dye across the wound. Looking under magnified cobalt blue light, either gross leakage from the defect or paling of the fluorescein dye wound indicate an active leak (indicating dilution of dye with intraocular fluid).
Suggestive signs:
- Severe 360º subconjunctival hemorrhage and/or chemosis (conjunctival edema)
- Flat, shallow or “deflated” looking anterior chamber compared to the fellow eye (always examine the other eye to rule out injury and for comparison)
- Teardrop pupil – an irregularly formed pupil (not round) often forms a point that clues you to where the rupture is it points in the direction of the prolapsed uvea.
- New or asymmetric cataract; dislocated lens material
- Motility defect in the affected eye
- CT scan (order CT scan of the “orbits” for thinner cuts through the globes and orbit) showing a globe that is not formed or round in comparison to the other eye
Treatment & Plan
Salient orders in the event of a suspicious or confirmed open globe include:
- Consult an ophthalmologist
- Shield the eye at all times except examination with something that vaults over the eye preventing any contact to the eye
- Make the patient 1) NPO (nil per os; nothing by mouth) to prepare for possible surgery, and 2) on bedrest with explicit instructions to avoid bending over, straining, or coughing
- Order broad spectrum antibiotics to prevent endophthalmitis and tetanus toxoid if the patient is overdue or has unclear immunization status
- Provide antiemetics and pain medication as needed
- CT scan of the brain and orbits are often indicated to rule out intraocular foreign bodies
References:
- Castellarin, A. A., & Pieramici, D. J. (2006). Open globe management. Comprehensive ophthalmology update, 8(3), 111-124.
- Ehlers, J. P., & Shah, C. P. (Eds.). (2008). The Wills eye manual: office and emergency room diagnosis and treatment of eye disease. Lippincott Williams & Wilkins.
- Harlan Jr, J. B., & Pieramici, D. J. (2002). Evaluation of patients with ocular trauma. Ophthalmology Clinics of North America, 15(2), 153-161.
- Seidel Test. Retrieved August 21, 2017, from http://eyewiki.org/Seidel_Test



